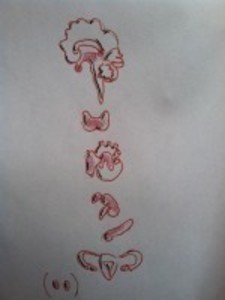
What Are Endocrine Disruptors?
The hormones in our bodies are regulated by the endocrine system and they impact a number of bodily functions, including metabolism, growth, and development. An endocrine disruptor is a chemical that disturbs the way the endocrine system normally functions, thereby interfering with the way hormones and the body functions, as well.
How Do Endocrine Disruptors Impact Women’s Health?
Scientists have found links between endocrine disruptors and a number of health problems in women. Since most studies have only tested animal responses, scientists cannot conclude that these compounds have the same impacts on humans, but most believe that they do.
The following are only some of the health issues that have been linked to endocrine disrupting chemicals:
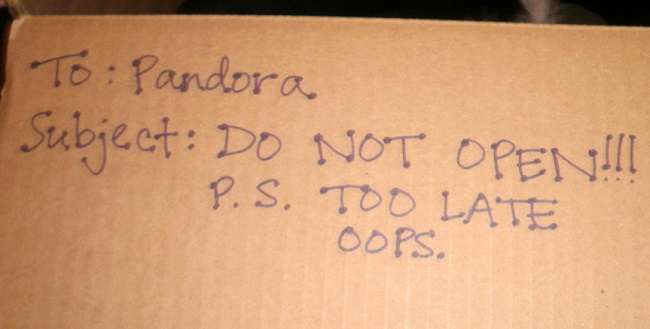
Precocious Puberty Possibly Due to Endocrine Disruptors
The early onset of puberty may be due to endocrine disrupting chemicals that are pervasive in the environment. The Journal of the American Academy of Pediatrics has found environmental toxins to be a possible explanation for precocious puberty.
While scientists are unsure if the early onset of puberty is due to endocrine disruptors or childhood obesity, it is important to note that endocrine disruptors also seem to cause insulin resistance, which can lead to weight gain.
Vaginal Cancer from Endocrine Disruptors
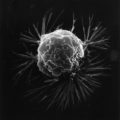
Unfortunately, there have been human cases that have shown a direct link between endocrine disruptors and the development of vaginal cancer.
Women took diethylstilbestrol (DES) to prevent miscarriages and morning sickness, only to find that this chemical caused their daughters to develop cancer, according to the Environmental Protection Agency. Scientists are still not exactly sure why DES caused vaginal cancer.
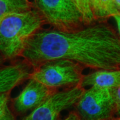
Endocrine Disruptors Tied to Breast Cancer
The EPA also acknowledges correlations between endocrine disruptors and certain cancers, such as breast cancer. A study published in Environmental Health Perspectives found environmental toxins increase breast cancer by affecting the regular development of breasts and mammary glands.
The Yale University School of Medicine bolsters this research, showing that endocrine disruptors increase a woman’s risk of breast cancer, particularly if she is exposed to such chemicals during embryonic development.
Endocrine Disruptors Impact Ovaries
The McLaughlin Center for Population Health Risk Assessment in Canada cited the increased risk of ovarian cancer from exposure to environmental toxins, such as pesticides and herbicides, noting that hormone levels seem to impact such outcomes.
The journal, Endocrine Reviews, reported that women with polycystic ovarian syndrome (PCOS) have higher levels of endocrine disruptors (specifically BPA) in their systems. PCOS is a disorder in which women, during their reproductive age, develop small cysts on their ovaries (in most cases). PCOS may impact a woman’s menstrual period, resulting in less frequent periods or none at all, and can make it difficult for a woman to become pregnant.
Uterine Disorders and Endocrine Disruptors
Endocrine disruptors have been found to reprogram genes in the uterus to grow uterine leiomyoma, or uterine tumors. Although these tumors are benign, they may cause heavy menstrual bleeding and/or lead to infertility.
The American Journal of Epidemiology has found links between the use of hair relaxers and uterine leiomyomata, suggesting that hair relaxers, used by many women, have endocrine disrupting chemicals.
The Society of Toxicology reported findings that mice exposed to high levels of genistein, a phytoestrogen found in soy products, developed uterine cancer later in life.
This same organization has shown connections between endometriosis, or the development of endometrial cells outside of the uterus, and endocrine disruptors, notably TCDD, a dioxin. The study found that endometrial cells do not properly respond to progesterone hormones when disrupted by TCDD, which can lead to endometriosis and sometimes infertility.
The Yale School of Medicine has found that endocrine disruptors block gene expression in the uterus, thereby disrupting the proper development of the uterus, which can lead to cancers, endometriosis, and infertility.
Endocrine Disrupting Chemicals Can Cause Infertility
Concentrated levels of hormone-mimicking chemicals can stop ovulation, just as contraceptive pills do, according to The Oxford Journals.
Polybrominated diphenylethers, chemicals used in fire retardants, are linked to cases of infertility. The Society of Toxicology has shown this chemical also reduces thyroid-stimulating hormones (THS) in pregnant women, which can negatively impact fetal brain development.
When Do Endocrine Disruptors Impact a Woman?
Most scientific findings emphasize that exposure to endocrine disruptors during rapid developmental periods, such as gestation, is more detrimental to a woman’s health than exposure at other times. In fact, the Federation of American Societies for Experimental Biology reported that endocrine disruptors often target the genes responsible for the development of an organism, interfering with the proper development of that organism.
Of course, this doesn’t mean that endocrine disruptors stop affecting us once we’re grown. The very chemicals that cause breast cancer have also been found to lessen the effectiveness of cancer fighting drugs. This is because most of the drugs used to treat breast cancer are made to reduce endogenous estrogens – which usually stimulate the cancer. While endocrine disruptors are just as effective as endogenous estrogens in stimulating the cancer, endocrine disruptors are not hindered by these drugs.
How Do We Limit Our Exposure to Endocrine Disruptors?
Endocrine Disruptors impact us every day, but we can limit the amount of toxic chemicals we absorb into our bodies by being aware of what these chemicals are and where they can be found. A good rule of thumb is to start cutting back on the processed goods in your life. If you have difficulty reducing the consumption of processed goods, just start with a few items and continue from there.
Not only do we ingest endocrine disruptors when we swallow pthalates in medication coatings, but we also wear them on our faces in the form of toxic cosmetics and contaminate our water sources with chemical toxins in widely used herbicides. Determine what are safe substitutes, like kitchen cosmetics or safe pesticide alternatives. Start small, choose wisely, and stay abreast of known endocrine disruptors.
Toxic Cosmetics
Kitchen Cosmetics
Is Your Deodorant Linked to Breast Cancer?
Phthalates in Medication Coatings
Endocrine Disrupters in the Environment:
Milk, it Does a Body Good?
Early Onset of Puberty
Could This be a Contributor to Weight Gain?
Chemical Toxins in Commonly Used Herbicides