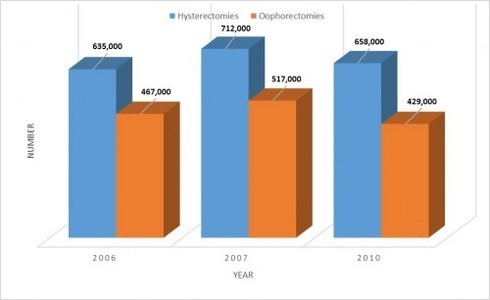
The hysterectomy and oophorectomy industry is growing annually with approximately 700,000 hysterectomies performed every year. The oophorectomy rate is about 70% of the hysterectomy rate. These are merely estimates based on a sample of inpatient data from short-term, acute-care, nonfederal hospitals along with hysterectomy and oophorectomy outpatient percentages published by the Agency for Healthcare Research and Quality (AHRQ). In 2003, 8.6% of hysterectomies were outpatient (ambulatory) according to Table 10 in this publication. In 2012, that rate was much higher at 39.8% as shown in the right-hand side bar here. And according to page 8 of the aforementioned publication, the 39.8% pertains to only abdominal and vaginal routes. The 2012 oophorectomy outpatient rate was 36.7% (bottom of page 7). The Centers for Disease Control (CDC) reports only inpatient hysterectomies which is why hysterectomy rates are typically understated by the media. A 40% understatement is a gross misrepresentation and outpatient hysterectomies now likely exceed 40%.
Hysterectomy is seen as panacea for a multitude of women’s health issues. Unfortunately, it is not, and yet, this perception that hysterectomy is a cure-all survives, largely because of false information from gynecologists, gynecologic oncologists, other medical professionals, hospitals, surgical centers, the media, and women who have had the surgery(ies). Below are some comments I have read and heard since my unwarranted hysterectomy. I am curious what other women were told before their surgeries.
What Gynecologists Say Before the Hysterectomy
- The uterus is just a useless, bleeding organ once you’ve completed your family.
- Well, you can’t continue with these problems.
- It’s time for that hysterectomy we’ve been discussing.
- You’ll wish you’d done it sooner.
- You’ll feel like a new woman.
- What’s your problem? A lot of women have hysterectomies.
- Sex won’t be any different; I’m not operating on your brain.
- Myomectomy won’t work. Your fibroids will come back and you’ll need another surgery.
- We can’t keep checking your lining and you don’t want uterine cancer. Let’s just get it out so you don’t have to worry about it.
- You should not be bleeding after menopause. (Fails to mention that most cases are nothing serious.)
- I’m removing the crib, not the playpen.
- You are close to menopause anyway.
- You don’t need your ovaries since you’re close to menopause (or in menopause).
- You may have cancer.
- You won’t have to worry about endometrial cancer. (Does not reveal how rare it is.)
- You won’t have to worry about cervical cancer. (Does not divulge that it is rare and takes years to develop from untreated abnormal cells.)
- You won’t have to worry about ovarian cancer. (Does not reveal how rare it is in women who do not have a genetic predisposition.)
- Everything has to come out.
- If you have a hysterectomy, you won’t have to take a progestin / progesterone. It will make HRT much easier.
What Gynecologists Say After the Hysterectomy
- You were a mess in there. It’s good we didn’t wait any longer.
- You are lucky you did not have cancer.
- No more worries about gynecologic cancer.
- That (problem) wasn’t caused by the surgery.
- We’ve never heard of that / those problems before.
- You can’t be having those symptoms…you still have your ovaries.
- None of my other patients have that problem. Maybe you need to see a psychiatrist.
- You are just depressed. Here’s a script for an anti-depressant.
- It’s all in your head.
- The patch works for all my other patients. I don’t know why it doesn’t work for you.
- You were already in menopause. You shouldn’t be having any symptoms.
- Your ovaries have nothing to do with your thyroid.
- I can’t help you anymore. You’ll need to find another doctor.
What Women Say About Hysterectomy
- You’ll be fine. You’ll just be a little tired for awhile.
- My husband can’t tell the difference during sex (but fails to divulge that sex is disappointing for her until after you’ve had surgery).
- I can have sex any time now…don’t have to worry about bleeding (but fails to mention she no longer has any interest / libido).
- I will save so much on pads and tampons! (She doesn’t realize she may very well trade those for incontinence supplies down the road since hysterectomy is associated with incontinence.)
- I’ll be fine once I balance my hormones.
- I’ve gained some weight but doesn’t everyone after menopause?
- It’s the best thing I’ve ever done. No more periods. Woo-hoo!
- I feel like a new woman.
- I wish I’d done it sooner.
Hysterectomy Facts: What No One Seems to Talk About
- Hysterectomy destroys a woman’s figure due to the loss of structural / skeletal support (citation).
- Hysterectomy compromises bladder and bowel function (see articles here and here).
- Hysterectomy increases risk of bladder and bowel prolapse (see articles here and here).
- Your vagina will likely prolapse over time (citation).
- Many women report a loss of sexual function (libido, arousal, response) regardless of whether or not ovaries are removed (see articles here and here).
- Hysterectomy is associated with an increased risk of heart disease even when ovaries are not removed (citation).
- Hysterectomy is associated with lower bone density even when ovaries are not removed (citation).
- Hysterectomy increases risk of thyroid cancer (citation).
- Hysterectomy is associated with a 30% increased relative risk of renal cell (kidney) cancer (citation).
- Hysterectomy is associated with reduced ovarian function or complete ovarian failure causing an increased risk for a number of health problems (citation).
- The ovaries of intact women produce hormones their whole lives and keep us healthy (citation).
- Gynecologic cancers are rare and account for only a small percentage of hysterectomies. If you look at the National Institutes of Health’s (NIH) cancer statistics, the 2015 estimate of new cases of cervical cancer is 12,900 and endometrial cancer is 54,870. This total of 67,770 accounts for just a small percentage of the 700,000 hysterectomies each year. The 2015 estimate of ovarian cancer is 21,290 with a woman’s lifetime risk being a measly 1.3% which does not justify the 450,000+ oophorectomies each year. According to this JAMA Surgery article on 2007 inpatient procedures, “Two operations on the female genital system, hysterectomy and oophorectomy, accounted for a total of 930,000 procedures (89.3% and 84.6%, respectively, were elective).” These figures do not include the roughly 300,000 outpatient hysterectomies and oophorectomies. Another procedure of the ob/gyn specialty, c-section, is reported as the “highest-frequency procedure in this list and accounted for $7.7 billion in aggregate costs.” Also concerning is that c-sections increased by 46% from 1997 to 2007. Oophorectomies decreased by 20% during that same time frame. The article does not say if hysterectomies increased or decreased. This points to long-standing overuse of harmful surgeries in the ob/gyn specialty.
- Graduate Medical Education requires that each resident do at least 70 hysterectomies. Organ sparing myomectomy (fibroid removal) and cystectomy (cyst removal) are not required procedures for gynecology residents (citation).
The Myth of the “Happy” Hysterectomy
I am always curious why women who claim to be happy with their hysterectomies hang out on hysterectomy forums. You would think they’d be out living life now that they are free of whatever gynecologic problems led to the surgery. Other types of surgeries don’t have dedicated forums and people posting long after their surgical recoveries. Surgeries are supposed to solve your problems so why would you need support and advice once you have recovered from the surgery?
Granted, some of the problems can take years to manifest. Others are more immediate such as loss of sexual function and hormonal / endocrine havoc if ovaries were removed or shut down shortly post-op. The skeletal changes that destroy our figures, backs, and hips are gradual but start to become evident within the first couple years. Many women don’t seem to realize (or maybe they are just in denial) especially if they gained a bit of weight. We can feel the changes before we see them. There are odd sensations (which are uncomfortable and maybe even painful) due to the bones and tissues (as well as bladder and bowel) shifting and migrating “south” via gravity. The figure changes are typically evident long before the chronic back, hip, and leg pain sets in from the shifting and misalignment of bones (ribs resting on the hip bones) and compression of nerves and blood vessels.
The bladder and bowel effects can be just as distressing and life-altering as detailed here. This Medscape article on the long-term effects of hysterectomy has several sections about impacts to pelvic organs (may require free registration to read full article). You can read more about the anatomical and skeletal effects of hysterectomy here. Even though I aged 15+ years in a matter of months after my hysterectomy, I am just as devastated by the disfigurement…maybe more so. And the bowel changes and loss of my sexual self are big losses too! This “Can Hysterectomies Hurt Sex Lives?” article talks about this after effect as well as others. This Medscape article states:
Even hysterectomy alone, for example, without the removal of the ovaries, can result in sexual dysfunction because of neurovascular injuries. Removal of the uterus and ligation of the arterial supply at the uterine pedicles can result in ovarian atrophy and fibrosis of the vaginal wall and clitoral cavernosal smooth muscle.
This “Evaluating Sexual Dysfunction in Women” article cites mechanisms of sexual dysfunction post-hysterectomy as follows:
Scar tissue may prevent full ballooning of the vagina, which makes intercourse more difficult. The loss of the uterus results in diminished total vasocongestion and the lack of uterine contractions, which may trouble some women. Internal scarring or nerve damage from the surgery may on occasion result in pain or lack of feeling during or after sexual intercourse.
The article also cites statistics from the Maine Women’s Health Study (see page 621) showing a significant increase in sexual dysfunction post-hysterectomy. Of the patients for which complete data was available, “no interest in sexual activity” increased from 49% pre-hysterectomy to 75% at 12 months post-hysterectomy. “No enjoyment of sexual activity” increased from 44% to 84%.
If you do some sleuthing, you will usually find these “happy hysterectomy” women posting elsewhere about problems they’ve developed since surgery such as mood and personality changes, weight gain, joint pain, fibromyalgia, bladder and bowel problems, sexual dysfunction, prolapsing vaginas, no longer feeling like a woman, poochy bellies, back, hip, and leg pain, bloating, sleep problems, nerve issues, vision changes, rapidly aging skin, thinning and graying hair, muscle wasting. They may go from doctor to doctor only to hear “well, you are getting older.”
Mood Changes Post Hysterectomy and Oophorectomy
The mood changes, especially for women who have had their ovaries removed, can be so severe they lead to suicide or thoughts of suicide (ideation). Even absent depression, many women report a blunting of emotions and loss of joy / vibrancy and interest in life. It’s as if all the color in life has changed to a blah gray. This article talks about these brain chemistry changes. It’s difficult for people to grasp or fathom how such drastic changes can result from a surgery that is so common to the point that 40% of women aged 45 to 54 have had one (4th paragraph). If you think about the fact that the uterus and ovaries are the very parts that make us female, it is no wonder we feel dead after their removal. If you think of the uterus as the only uniquely female organ (since the testicles are a man’s equivalent of the ovaries), that may explain why women who keep their ovaries oftentimes complain of blunted emotions and loss of femininity.
Also of note in the article on brain chemistry changes is that women tend to never forget the date of their hysterectomies. It is that life-altering! For women who do not connect the dots, it can be a big aha! moment when they finally do. But we still can’t, for the most part, count on them to warn intact women. After probing, some women do eventually admit they regret having had the surgery. But those who “sing the praises” early post-op seldom admit to regret once the problems set in. Granted, some women’s gynecologic problems, especially those involving chronic pelvic pain, are so severe that the long-term trade-offs of hysterectomy are worth it. Endometriosis is one such condition; however, hysterectomy and/or oophorectomy is not a cure so the pain may continue or return.
Financial Interests Disguised as Support
To make matters worse, many of the hysterectomy forums are sponsored by device companies, and thus, have deep conflicts of interest. One of the larger forums, has drawn the attention of a former New York Times reporter for their questionable presentation of hysterectomy information. Here she discusses the deep conflicts of interest between the site’s founder and the parent company, Intuitive Surgical, and their promotion of the da Vinci robot, a surgical tool.
On these particular forums, negative comments are censored, posts about hysterectomy’s effects on a woman’s figure are deleted and post-hysterectomy ovarian failure is represented as if it is natural menopause. It is not. Even more disturbing is the manner in which they present hysterectomy. For all intents and purposes, hysterectomy is a perfect solution.
I always wonder too what’s with women who ask for input or advice and then attack those who share their negative experiences and try to warn them about the many risks and long-term effects. Why is that? We are only trying to save you from a life of never-ending heartache and health problems.
The fact that the “sister”hood site has so many sub-forums – HRT, no HRT, sexual dysfunction, pelvic floor and bladder issues, the road less traveled (long-term problems), separate surgeries, return of endometriosis, aching hearts – is a huge red flag that hysterectomy is typically fraught with more problems than it solves. And some of those problems are permanent and progressive. That is why you see women posting many years after their surgeries even though they may have been “singing its praises” early post-op.
A Surgical Racket
Wake up ladies! We are kidding ourselves if we think physicians don’t remove organs unnecessarily. Or that they are upfront about the negative effects. Is it possible some of them are not aware of the after effects? I suppose that could be the case if they aren’t taught in medical school. But surely any doctor who has been doing hysterectomies and/or oophorectomies for years has to see the harm. And the studies prove these surgeries are harmful. They would have to put their heads in the sand to not see it. So often, women are neither advised about all of the treatment options, surgical and non-surgical, nor fully informed of the risks and benefits of those options. As Dr. Ernst Bartsich, former Clinical Associate Professor of Ob/Gyn at New York Weill Cornell Medical Center, says in “Hysterectomy: The Operation Women May Not Need” women would not choose hysterectomy if they knew the “dramatic and life-altering” consequences.
Another gynecologist who has been outspoken about the deception and overuse of hysterectomy is Dr. Stanley West, author of “The Hysterectomy Hoax.” He talks about how gynecologists are urged to cultivate their patients for the ultimate revenue producing treatment, hysterectomy, in this article “Far Too Many Hysterectomies Still Being Performed.” He is quoted as saying:
It is time we doctors stopped disassembling healthy women. But nothing will change until more women look their doctors in the eye and calmly state their determination to remain intact women.
Another noted gynecologist who appeared on Dr. Oz said that the mantra at Tufts when she was chief resident was:
There is no room in the tomb for the womb.
This article calls out the absurdity of gynecologists treating the uterus as a “useless, bleeding, symptom-producing, potentially cancer-bearing organ” that needs to be prophylactically removed once women have completed their families. Here the uterus is called “a terrible thing to waste.”
This “Unnecessary Hysterectomy: Lack of Informed Consent” article delves into the profit motives of the healthcare industry, lack of regulation of medical professionals, and the public’s misguided belief that medical professionals are ethical and competent. These factors coupled with sexual prejudices and women’s ignorance about their bodies makes women even more vulnerable to medical abuse.
The lure of “less invasive” surgical methods (laparoscopic, robotic) is just another marketing ploy to get women into the operating room. Sure, the smaller incisions are a plus but the same amount of cutting and damage happens internally so the long-term effects are the same as traditional / “more invasive” methods. Dr. Ernst Bartsich is quoted in this Health Day article about the overuse of hysterectomy and how discussions about the surgical methods distract from the issue that hysterectomy is rarely necessary. Unfortunately, we cannot count on our government to address this over-treatment and harm. I recall reading of someone being told by a legislator that it would put too many gynecologists out of business. Another legislator said that Congress does not legislate healthcare because it is a “slippery slope.” There have been two Congressional hearings on the overuse of hysterectomy, one in 1978 and one in 1993 but still the problem persists. The healthcare providers member organizations (e.g., ACOG, AMA) have very powerful lobby efforts / Political Action Committees (PAC’s). Their political action websites, Ob-GynPAC and AMPAC, can be found here and here, respectively. The full gamut of ACOG’s advocacy efforts can be found here. The following quote by Upton Sinclair explains it in a nutshell:
It is difficult to get a man to understand something when his salary depends on his not understanding it.
Three of the most overused surgeries – c-section, hysterectomy, and oophorectomy – belong to the ob/gyn specialty. And even though c-section has been added to ACOG’s Choosing Wisely list of overused tests and procedures, hysterectomy and oophorectomy are not on the list. Notice too that the Patient List includes only one of the five items from the Clinician List. Is ACOG trying to keep patients in the dark? Ironically, clinicians are advised not to screen for ovarian cancer in asymptomatic women at average risk. Yet, gynecologists are removing women’s healthy ovaries at alarming rates!
You would think women’s organizations would want to take on the issue of unnecessary female organ removal. But the only one that has is the HERS Foundation which was founded in the early 1980’s to educate the public about the critical lifelong functions of the female organs. Women who have undergone hysterectomy and/or oophorectomy reported these adverse effects. HERS also provides information on treatment alternatives. This 12 minute video of female anatomy and the functions of the female organs is eye-opening.
Efforts by me and others to engage National Organization for Women (NOW) and National Women’s Health Network (NWHN) have not been acknowledged. The mission of these two organizations is deeply rooted in reproductive choice so they may view the issue of unnecessary hysterectomies and oophorectomies as counter to a woman’s choice. However, by not recognizing the gross overuse and failure by doctors to fully disclose the harm and treatment alternatives, they effectively limit the very reproductive choice they seek to promote.
I will say that at least NWHN strongly discourages women from undergoing hysterectomy on its Hysterectomy Fact Sheet. But why then does it give so much more press to hysterectomy than treatment alternatives? The Fact Sheet gets mired down in questions to ask your doctor about hysterectomy and a detailed explanation of each surgical method when it should be focusing on conditions and treatment alternatives. At least they list the HERS Foundation as a resource. But it’s concerning that they also list Hystersisters. Menopause Hormone Therapy is one of their Advocacy Issues presented as “a triumph of marketing over science and advertising over common sense.” Hysterectomy is also much more about marketing than science and common sense! NWHN states that menopause is a normal transition versus a disease that needs to be treated with drugs. There would be much less need for hormone therapy if there weren’t so many hysterectomies and oophorectomies!
You May Be A Guinea Pig
Did you know that many of the unnecessary hysterectomies are done for training purposes? Gynecology residents in accredited Graduate Medical Education (GME) programs must do a minimum of 70 hysterectomies. Not only that, you may be surprised to learn (as late as the day of surgery) that “your” hospital is a teaching facility despite no university affiliation, the big Mercy system included. With a woman’s lifetime risk of all gynecologic cancers being less than 3%, it is obvious that the removal of female organs is rarely necessary. So why have nearly 40 percent of women aged 45–54 had a hysterectomy? We should also question why the oophorectomy (ovary removal / castration) rate is as high as 73% of the hysterectomy rate as shown in the chart below.
The average woman’s lifetime risk of ovarian cancer is very low at 1.3% and history has shown that ovary removal has not reduced ovarian cancer deaths. Not only that, studies have clearly shown that ovary removal even after menopause is associated with many increased health risks – heart disease, osteoporosis, dementia, Parkinson’s, depression, anxiety, lung cancer to name just a handful. You can see all the studies here. Of course, these risks also apply to women whose ovaries fail after hysterectomy since the ovaries are essential for good health.
Naturally menopausal ovaries continue to produce hormones from the inner stroma as mentioned in this article and hysterectomy with ovarian conservation is associated with reduced ovarian function. Female organ removal is a very lucrative business and no one seems to care about all these unnecessary surgeries that are causing so much harm to over 700,000 women every year.
To All Intact Women Out There
Be on your guard…you could be next.
- Make sure you get a definitive diagnosis and do your own research on all of your treatment options and their risks and benefits.
- Be wary of any procedure that alters the “reproductive” system (hysterectomy, unilateral or bilateral ovary and/or tube removal, ablation, tubal sterilization). Even ablation that is sold as a hysterectomy alternative can do just the opposite – increase your risk for hysterectomy as explained here.
- Keep in mind that with hysterectomy and/or oophorectomy you may be trading temporary (gynecologic) problems for the permanent and progressive problems caused by these surgeries.
- Don’t be lured in by the “minimally invasive” sales gimmick, the “sister”hood, or cancer scare tactics. The high rate of hysterectomies leads women to falsely believe that it is a benign surgery.
- If you are still considering hysterectomy, keep in mind that actions speak louder than words. Be observant of women who’ve had hysterectomies. If you knew them before surgery, you can oftentimes tell they have changed, if not in their looks at least in their demeanor / disposition. If they are a number of years post-op, they will have that altered figure with the thick and shortened midsection.
- Don’t shortchange yourself (or your significant other). You deserve to remain whole. There may be other options available but you will likely have to seek them out. I fell into that trap. Here is my story.
For Women Who Have Had Hysterectomies
- Make sure you understand the repercussions of organ removal so you can make the best health decisions for your altered body.
- Do not make excuses for doctors who remove organs unnecessarily and are not honest with their patients. We deserve better!
- Be honest about how the removal of your organ(s) has affected your life and health. Share what you have learned about the life long functions of the uterus and ovaries. We need to stop treating hysterectomy as a surgery that most women are expected to have as a sort of rite of passage. It is only through open and honest communication that we can make a difference going forward.
- Tell your story to various organizations. You can do it here on Hormones Matter. Consumers Union (a subsidiary of Consumer Reports) and ProPublica have patient safety projects. You can submit your story to CU’s Doctor Accountability and Medical Errors. ProPublica’s Patient Harm form can be found here.
In conclusion, most hysterectomies and oophorectomies are unnecessary and there is plenty of evidence that many women are conned into getting these damaging procedures. As women, we need to see through the con and protect ourselves and other women. These surgeries have risks and long term consequences. Here is how the con worked on me. I am curious what you were told by doctors and other women before your surgery. Please share. You can find all my articles about hysterectomy here.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by National Cancer Institute on Unsplash.