A persistent notion in medicine is that the only time mitochondria precipitate, or in any way influence illness, is when mDNA mutations are involved and/or with frank starvation. Absent those two events, the magical mitochondria will keep chugging along and there is no need to consider their impact on health or disease. This belief emanates partly from another all-too-persistent notion that holds tightly to a compartmentalized model of organismal function, suggesting that each bodily system and thus each disease process is unique and distinctly separate from everything else, and partly from the way most folks are taught about mitochondria – by rote memorization of the Krebs cycle. As a result and except in specific circumstances, most physicians and many researchers see no role for mitochondria in health or disease.
This is true with COVID as well. Even though COVID presents disparately across patient populations, is clearly not limited by body compartment or system, and not only does not fit within any diagnostic model to date but shatters everything we think we know about illness, folks are reticent, nay adamant, that mitochondria are not involved. COVID is not a mitochondrial illness, they proclaim. To that end, on a somewhat regular basis, I see posts, threads, and comments about just how unimportant mitochondria are to COVID and really, to health in general.
Stressed Mitochondria, Inflammation, and COVID
Some months ago, a gentleman argued that the chronic inflammation caused by COVID was related solely to altered immune function similar to that seen in conditions like rheumatoid arthritis or lupus. He went on to say that he did not see any role for mitochondria in this. Similarly, another gentleman was equally adamant that there was no known relationship between “mitochondrial health impacting which immune response or pathway will be activated.” He argued further that my suggestion of stressed mitochondria triggering the inflammatory responses seen in COVID-related blood pressure drops and cytokine storms was not possible per the tenets of modern immunology. It was foolhardy for me to consider otherwise.
Beyond the obvious faceplant response – ‘as if the immune system could function without the help of the mitochondria; as if anything could function without the mitochondria’ – there is an ample amount of research linking mitochondrial function to immune function predating COVID and a burgeoning body of research linking mitochondrial response to COVID severity. Indeed, some of the more recent research suggests that not only does SARS- COV2, the viral protein associated with COVID directly influence mitochondrial function like many other viruses do, but also that it is only the host variables e.g. mitochondrial fitness that determine how far the virus is allowed to progress. Mitochondria, it appears, are the determining factor of illness severity, something I have been saying since the beginning of this pandemic.
When this particular series of ‘COVID does not involve the mitochondria’ comments came up, I was speaking about the hijacking of the mTOR pathway by other viruses and speculating as to whether COVID might do the same. The mTOR pathway includes a set of enzymes that regulate cell and mitochondrial metabolism via multiple mechanisms. Though mTOR are not mitochondrial proteins, as they are located in the cytosol adjacent to another set of organelles called lysosomes, they provide critical signaling to mitochondria involving energy metabolism and stress response. In fact, mTOR coordinate mitochondrial energy consumption and production. They initiate these nutrient signals by binding or unbinding themselves to the lysosomes. Among those signals that mTOR respond to is protein or amino acid status. Low protein effectively inhibits mTOR enzymes. Absent outright starvation, which is entirely possible in critical illness, protein metabolism is dependent upon mitochondrial function. Specifically, protein catabolism and synthesis both require energy or ATP, which in turn requires an array of micronutrient co-factors to power mitochondrial enzymes, the machinery involved in these processes.
Returning to the claim that the COVID cytokine response was akin to the autoimmune diseases like arthritis or lupus, that claim is absolutely correct. The response is akin to one of an autoimmune disease process, but what most fail to recognize is that autoimmune disease process is itself tied to the mitochondria, through multiple channels, including mTOR. Since these conversations arose from a post on viral hijacking of mTOR and the inflammatory patterns observed with autoimmunity, let us dig into those relationships.
Th-17 Cells, mTOR and the Mitochondria
Common to both the severe and long COVID and autoimmune illness, are hyperactive pro-inflammatory Th17 cells with underactive anti-inflammatory Treg cells. Th17 modulation is tied to mitochondrial fitness. The Th17 response is thiamine dependent. Thiamine is the rate limiting co-factor to key enzymes involved in mitochondrial energy production, including those at the entry points for the glucose, fatty acid, and amino acid pathways and other enzymes within the TCA/Krebs cycle. Thiamine deficiency derails mitochondrial energy production, shifting it from oxidative phosphorylation and towards aerobic and eventually, anaerobic glycolysis. Even aerobic glycolysis, however, is thiamine dependent. These shifts in energy production are mitochondrial danger signals to the immune cells, including Th17 proinflammatory response. The mTOR proteins, are also involved. When oxidative phosphorylation, glutamine metabolism, and fatty acid synthesis, all which are thiamine dependent, are lagging and energy wanes (e.g. with insufficient thiamine or other mitochondrial nutrients), mTORs energy metabolism becomes anaerobic and pro-inflammatory – e.g. Th17s upregulate and the anti-inflammatory Treg cells downregulate.
Renowned mitochondrial researcher Robert Naviaux would tell us that in both autoimmunity, and in COVID, particularly Long COVID, the mitochondria are stuck in battleship mode; that they lack the energy not only to complete the tasks at hand, but to create more energy. Dr. Lonsdale would tell us that this is because the mitochondria lack the sufficient nutrients to convert food into energy, especially thiamine. From our book, notice how many times thiamine, vitamin B1, is required. Notice also, how many other micronutrients are required to convert food substrates, glucose, proteins, and fatty acids into ATP.
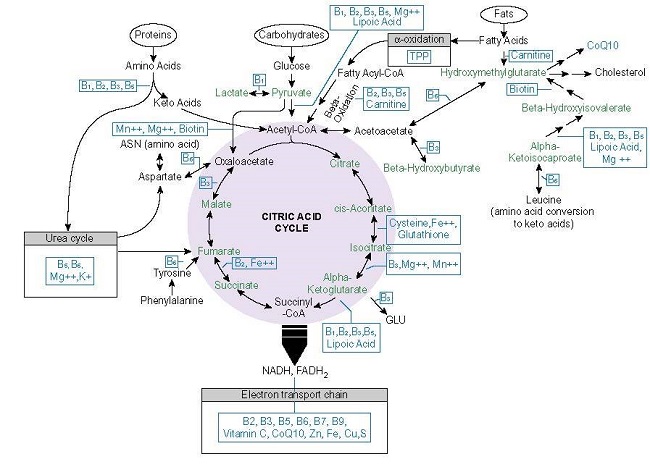
Now consider the high calorie, low nutrient composition of the modern American diet, the metabolic dysfunction associated with the severity and chronicity of COVID, and the range of inflammatory disorders afflicting many of the patients who develop severe and/or long COVID. These are connections that must be recognized.
We know that absent sufficient mitochondrial nutrients, energy wanes. When energy wanes, inflammatory cascades remain unchecked; among them, hyperactive pro-inflammatory Th17 and underactive anti-inflammatory Treg cells. We have to consider also that although pharmaceutical interventions may abrogate that inflammation superficially and temporarily, they do nothing resolve the underlying issue, which is micronutrient deficiency. Since most, if not all, medications damage mitochondria by one mechanism or another, their use, while necessary in some instances, ultimately imperil mitochondrial capacity and exacerbate any underlying energy deficiency as well. So, when we look at folks most at risk for the more severe cases of COVID and/or those who develop symptoms consistent with Long COVID, it is important address the inflammatory response caused by the lack of sufficient energy.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.