In using a fictitious example, the mother of a football playing athlete takes an interest in a head injury sustained by her son. Perhaps she wanted to know why he developed certain symptoms and what sort of treatment might be helpful. Doing her own research, she has been confronted with a mysterious, often repeated, discussion about “free oxygen radicals” in the brain in relation to head injury. This post may hopefully take some of the mystery out of the discussion and even suggest a means of prevention.
Burning a Fuel Is Oxidation
The chemistry of energy metabolism as it affects the brain/body is exceedingly complex. However, in order to illustrate the principles of oxidation (burning) perhaps, it can be seen in the simplest terms by recognizing what happens when we burn (or oxidize) something such as a sheet of paper. The paper does not ignite spontaneously: some form of energy has to set it alight. When we strike a match, energy is consumed by the arm and hand of the person that does the striking. This energy is used to move the match against a rough surface and the friction causes heat energy to arise and light the match. Energy is required for each step. Having applied the flame from the match to the newspaper, we have transferred the energy and the match is incompletely burned. In each case, the match and the paper act as fuel, and the heat energy released is produced by the fuel combining with oxygen. Because of incomplete combustion, both the paper and the match are converted into ash, the leftover unburned portions.
Speed of the Oxidation
In this simple case, the heat energy is released into the atmosphere and disperses. The energy cannot be used to perform work. The same thing happens with an open fire but there is an additional factor. For example, if we blow on it, the fire burns more briskly. Sparks are produced that may set fire to the surrounding dead grass. Energy has to be captured and controlled to do work. Any form of burning, combustion, fire, or singeing (we have many words for the process) is produced by a fuel combining with oxygen. The resultant energy is used to do work. Combustion is never complete; some form of ash is left over.
In the body, we burn glucose and the term used is oxidation. The “ash” is carbon dioxide and water, both of which are partially lost in the breath. It is the speed of the reaction that makes a difference in the rate of energy production. Singeing is a very slow combination of the material with oxygen whereas an explosion is an extremely fast reaction. Neither of them could function without oxygen. The production of sparks from an open fire may be used as an analogy for free oxygen radicals. This part of the post may be overkill, but I am discussing everyday phenomena that are frequently taken for granted. Little or no thought is generally given to the mechanisms involved.
What Are Free Oxygen Radicals?
I have already compared them with sparks from an open fire. This means that oxidation in the body can be slow or fast and the speed of the reaction has to be controlled. Too little oxygen is as bad as too much, encapsulated as “all things in moderation”, arguably the most important philosophical annotation that has ever been conceived, since it applies to everything.
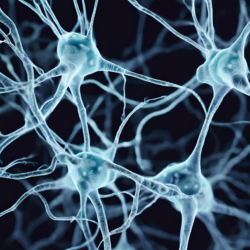
As already indicated, glucose is the major fuel of the body, particularly for the brain. The oxidation of glucose is mediated through a series of vitally important enzymes, yielding energy that is stored in the cell as a chemical substance known as ATP (adenosine triphosphate). An inexact analogy would be that a head injury acts as a form of stress that requires a vast amount of energy consumption to adapt to the injury. The rapid oxidation that follows gives rise to free oxygen radicals that are the equivalent of sparks in a vigorously burning fire. The “sparks” are thrown out of the “fireplace” in the cell and “set fire” (oxidize) to surrounding tissues, thus causing the damage. It is often difficult for people to understand that the energy required to give rise to mental and physical function is from a form of combustion induced by chemical reactions. The chemical energy has to be transduced to electrical and is the reason why we can measure the activity of a given organ such as the heart by the electrocardiogram and the brain by the electroencephalogram.
Note that oxidation does not occur spontaneously. The glucose must be “ignited” and vitamins are the equivalent of a match. Although it is a poor analogy, vitamins liberate and transfer energy. It is of course extremely important to recognize that energy is something that we cannot perceive in any way except by its effects. We cannot see heat energy but we can feel its effects. We cannot perceive the energy that drives the brain although we can appreciate the thoughts that arise from its consumption.
When we eat food it becomes the fuel that has to be oxidized, releasing chemical energy. That chemical energy has to be transduced to electrical energy to drive function. It must be stated that our bodies are constructed according to a code known as DNA. If that is imperfect, we may have “a genetic effect” responsible for disease. In addition, if the food does not contain the right fuel or does not contain the factors that ignite it, the effect is disease. The central figure is energy. Symptoms are sensory effects in the brain that indicate that “something is wrong (for example) in your left elbow”. Pain is felt in the brain, not the part of the body with inflammation. A genetic error may not initiate disease by itself. It often requires nutrient deficiency and/or some kind of stress such as an infection, trauma, or prolonged mental stress. Any one of these requires increased energy expenditure to adapt to the stress, in much the same way that a car uses more energy derived from fuel consumption when climbing a hill.
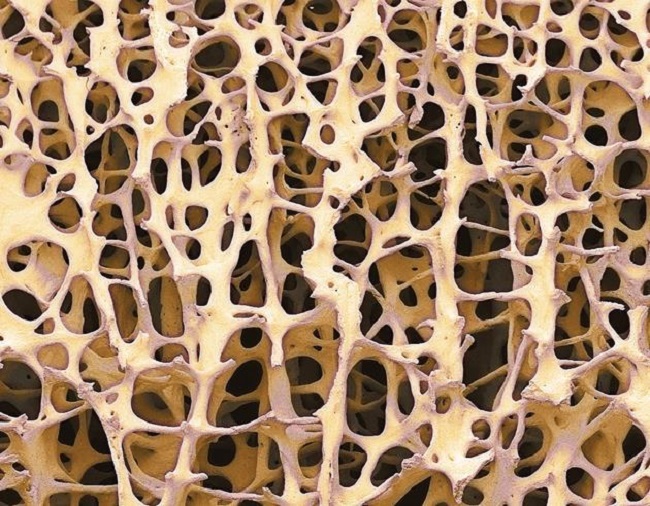
Traumatic Brain Injury
Traumatic brain injury is a significant cause of death and disability. The primary impact causes initial tissue damage which initiates biochemical cascades known as secondary injury. Free radicals are implicated as major contributors to secondary injury. Another manuscript reports a study on rats. These authors induced thiamine deficiency and found that there was an increase in free radicals in the brain. Exercise stresses body chemistry that depends on thiamine, riboflavin, and vitamin B-6. The requirements for these vitamins may be increased in active individuals, particularly athletes. Biochemical evidence of these deficiencies in active individuals has been reported, but studies examining these issues are limited and equivocal. There are no metabolic studies that have compared thiamine status in active and sedentary persons. These authors state that exercise appears to decrease nutrient status even further in active individuals with pre-existing marginal vitamin intakes or marginal body stores. Thus, active individuals who make poor dietary choices are at greater risk.
The ability of humans to respond to stresses, such as altitude, heat, trauma, surgery, or infection can be influenced by nutritional status. Hans Selye is the most famous scientist who studied the effects of physical stress on animals. He came to the conclusion that energy was necessary for the animal to meet the demands (adapt) imposed by any form of stress and that it was energy failure that was responsible for the animal’s collapse. He formulated the idea that chronic human diseases were the “diseases of adaptation”, implying energy insufficiency as the underlying cause. This suggests that the acute phase of an infection is the defensive, adaptive reaction that requires nutritional perfection to supply the energy.
Protection Versus Treatment
Currently, the only method to try to prevent brain injury in athletes is protective equipment and the statistics indicate that this does not seem to be very effective. That nutritional elements might have a protective effect on brain injury might seem like an absurd disconnect. We have repeatedly emphasized on this website that food choices are poor in the modern world. The diet for many people is laced with empty calories that challenge and overwhelm the mechanisms that govern oxidation. The vitamin content may be adequate for a well-chosen diet of natural foods but inadequate in relation to the empty calories, a state that is commonly present in young people in particular. We are well aware that measuring the concentration of thiamine in the blood, the usual and customary practice of attempting to identify thiamine deficiency is usually perfectly normal in mild to moderate deficiency. If our resolute hedonism causes us to continue making poor choices, perhaps it would make sense to add vitamins as supplements, an idea that has been castigated many times in published statements. This is because it is widely believed that “vitamin deficiency” in an advanced country like America is nonexistent. Finally, I must say something about treatment. There is some evidence that intravenous infusion of water-soluble vitamins given to an athlete that suffers from the symptoms of brain injury can be at least partially relieved. This is basically because these vitamins play a vital part in controlling the use of oxygen in cellular function. Without understanding these basic mechanisms, the use of intravenous vitamins to treat brain injury would be incomprehensible.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on June 7, 2018.
Image created using Canva AI.











Derrick thank you so much for all the information you share, I can’t stop reading every article. When I got my energy back by taking thiamine… I came to the conclusion that an energy deficit was causing me a very big medical symptoms chart… and the key was simple… energy! Upon recovering it, the entire mental and physical medical symptoms chart disappeared…And then I found your blog and I can connect so many loose ends, and it all makes so much sense!
I would like to ask you a question. Do you think that the sensory hypersensitivity (auditory, tactile, visual, etc.) that some people have, especially some children with neurodevelopment problems, could be related to a thiamine deficiency? Would this be a bad adaptation to the environment?
On the other hand, I have lived very “tired” all my life, since I was little. I’ve had good energy for maybe 4 months since I started taking thiamine. But if one day I consume a lot of carbohydrates, the next day I feel the abdomen (especially) and the muscles weak, and very tired. Could this mean that I need to take daily thiamine “forever”? By taking the supplement, it’s so perfect, it only takes minutes to kick in and I can pull myself together. Life seems very easy with energy! I say this after having lived 36 years tired! Thank you so much!
Sensory hypersensitivity is typical of thiamine deficiency
Thank you! It’s all I wanted to hear after 3 years looking for the cause! I refuse to believe that sensory disorders are inherited and we have to be like that. I hope to be able to tell you in a few months that everything has gone for the better with my son. I have read many of your posts and I continue reading in my free moments. I have put all my chips on the thiamine deficiency in my son, everything fits perfectly, I just have to wait for it to work its magic! In me it has already done it. We need you 100 more years on this plane. Health ♡
Hi, Dr Lonsdale.
Thanks for all the work you do.
B1 helps me a lot, but makes me smell weird. Is there a solution to this?
Do you know Dr. Cusack’s work on vitamins for TBI and ICP in the ICU? I have only heard of it second and third hand.
No
I meant Dr. Coimbra anyway. Sorry for the brain fog. I had been reading about Dr. Coimbra’s vitamin-based autoimmune protocol the same day as I was reading about Deborah Cusack’s connective tissue supplement recommendations. It seems that many people starting from different problems are converging on similar solutions (nutrition).
Yes, a medical revolution
Could Benfotiamine in conjunction with a high thiamine hcl dose (2000mg) cross the BBB more easily or at least thiamine generated from the Benfotiamine do so? My succinic acid I believe was low on a Nutri eval test in the step of that cycle but I am not sure what that indicates. I was curious what urine tests would reveal more information as well. Thanks for all your continued research.
The simple answer is that I don’t know!
Benfotiamine and even high dose Thiamin HCL can cross BBB to some degree, but not as effectively as B1 TTFD and Sulbutimine do.
Hello Dr. Lonsdale
Thank you for all your research into thiamine and its effects, they are life saving for many of us
I read recently that generation of TPP is dependant on the activity of DHFR, so if intracellular level of folate is low then TPP is not generated even when adequate thiamine is available.
Is it related to some paradoxal reactions of thiamine refeeding? Should folate be supplemented with thiamine to ensure proper TPP synthesis? It seems that DHFR activity is quite variable from person to person and could be an important factor in thiamine methabolism.
I also wonder if things like lithium orotate, which suppose to increase uptake of folate into CSF could be helpful in normalizing thiamine status quicker.
Thank you
Regards
Sergey
Dihydrofolate reductase is an enzyme that activates folate. Since it consumes energy it is dependent on thiamine pyrophosphate because that is cofactor to enzymes that produce energy. I think that you have it backwards!! It has nothing to do with thiamin refeeding. We have hypothesized, from clinical evidence, that thiamin deficiency results in energy deficiency and inactive folate and B12 concentrations are increased in the blood. When thiamin is given to the patient, B12 and folatre concentrations become normal. High folate and B12 concentrations in pregnancy have been reported to foretell the incidence of autism in the infant during infancy, thus supporting the evidence for thiamin deficiency as a cause of autism.
Thank you for your reply! Yes, I understand that increased ATP supply would deplete folate and B12 due to activation of methylation pathways.
However, I found several articles which also mention that reduced DHFR activity impacts TPP regeneration due to reduction of available NADH:
“At the cellular level, a folate deficiency may cause an indirect thiamine deficiency. Even though thiamine is present, it cannot be activated to thiamine pyrophosphate– its biologically active form–due to a deficient dihydrofolate reductase activity.[4,5] It is possible that the clinical features of a folate-deficiency neuropathy may be partly caused by indirect thiamine deficiency.”
“folate deficiency causes thiamine deficiency (thiamine regenerated via proton donation from NADH -> folate required to have enough dihydrofolate reductase to regenerate NADH)”
Also, it seems that reduced folate carriers are responsible for some of the processes in thiamine transport, and their activity is drastically reduced in folate deficiency.
So I hypothesised that low blood/CSF folate can aggravate thiamine deficiency via multiple routes and could be one of the biochemical blocks which should be addressed.
Folinic acid seem to induce DHFR activity and also provide enough folate to rescue reduced folate carrier activity.
I am sure that some of my problems (or all of them) are caused by thiamine deficiency/dependency (thank you once again for all your research and knowledge). I also have very low blood level of folate due to dietary insufficiency and curios whether it can disrupt my thiamine status even further.
Regards,
Sergey
You may be right. I don’t know