I never thought I would be an advocate for pain medication access. I have been clean from alcohol and non-opiate drug abuse for 17 years. I am an active member of a 12 step fellowship. I sponsor women and have a sponsor. I regularly attend meetings. For most of my recovery I was anti-pain medication. I still believe opioid pain medication should be avoided in most situations. I also advocated against pain medication—so that it would not get into the hands of teens.
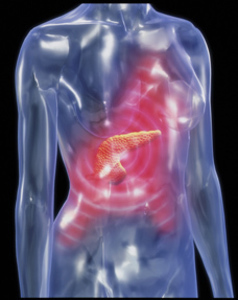
From Sphincter of Oddi Dysfunction To Chronic Pancreatitis
I dealt with sphincter of oddi dysfunction pain for over 13 years, never taking opioid pain medication for this condition. I also have painful neuropathy for which non-narcotic medication did not help. I chose to treat with alternative therapies, which sometimes helped. This year I was diagnosed with chronic pancreatitis. Chronic pancreatitis is well documented in the medical literature as being “excruciating”, “severe”, and even “miserable”. Some medical articles have documented chronic pancreatitis pain as worse than pancreatic cancer pain. In some states I qualify for palliative care, one step down from hospice care. There are no evidence-based treatments for chronic pancreatitis pain other than opioid pain medication and total pancreatectomy (pancreas removal).
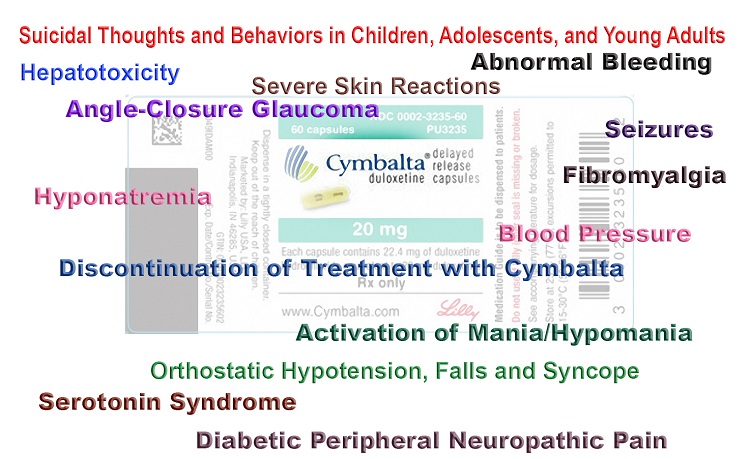
The horrible unrelenting pain flares drove my family and me to seek pain management. After all, I wanted to die. I am not just saying I wanted to die. I mean I really wanted to die. The pain was on par with labor pain. Imagine trying to function every day in labor—but have no break in between contractions? I learned to function with the daily pain but when the flares came on I thought I would die and if I didn’t I surely needed to figure out how to end my life and suffering. My primary care doctor and a gastroenterologist I later fired tried me on the usual first line treatments for pain. NSAIDs gave me microscopic colitis. Tylenol was useless. Non-cholinergics like amitriptyline caused severe itching in places I’d rather not mention. Nerve medications like gabapentin and Lyrica and anything affecting GABA caused flu-like symptoms and exacerbated my pancreatic symptoms (pancreatitis is a side effect). I tried hypnotherapy, acupuncture, reiki, yoga, meditation, magnesium, and any natural remedy I came across.
Eventually pain of this level wears on the body and mind no matter how hard you are working at treating it. Finally, after heavy consult with my Higher Power, sponsor, mom, husband, and a close recovery friend, it was decided I needed to actively seek stronger more effective pain relief. My primary care and pretty much all primary care doctors in my area have a policy of not prescribing opioid pain medication. Specialists, unless you have cancer, don’t either. No pain management doctor in our area who takes insurance will prescribe pain meds anymore—they only offer injections, procedures, and non-narcotic medications. At one point I relented out of desperation to have a celiac plexus nerve block. The pain doctor kept insisting it was the only thing that worked for pancreatic pain. My primary care totally bought into it too, mostly I felt because he didn’t have to write a prescription. These doctors had no clue how tapped in I was with research. Nowhere was it documented to be a proven treatment for chronic pancreatitis. Regardless, because I was desperate for pain relief and told this was my only hope, I paid a hefty copay, spent half the day in the hospital, was sedated and had a needle stuck through my abdomen. It did nothing. No relief.
A Near Stroke from Severe Pancreatitis Pain
At one point my body just could not handle the pain anymore. I had gone so long suffering that it said, “enough.” One evening a few months ago the pain intensified to a degree my blood pressure doubled (I have one of those little machines) and my right side went numb. I was about to have a stroke! From pain! Luckily I was saved with emergency pain medication. At this point my gastroenterologist was infuriated my primary or any pain doctor would not try to manage this. He ended up prescribing a low but effective dose of an opioid for the flares so I wouldn’t stroke out and die. Unfortunately, the hospital he worked at told him I needed to find pain management. I finally found a doctor quite a drive away who I have to pay out of pocket because apparently insurance companies think they are the DEA now and don’t want to approve insurance for pain doctors who prescribe opioids. For now, I have a safety net. I do not enjoy pain medication and only take when I absolutely need to. My recovering addict friends don’t get it and quite frankly they don’t have to. Try walking in my shoes, having chronic pain and illness for four years straight. Trust me, the only pill you’ll desire is one that makes you feel normal, not one with side effects.
Guidelines on Pain Management Ignore Chronic Pain
When the opportunity arose to comment on the draft Center for Disease Control’s “CDC Guideline for Prescribing Opioids for Chronic Pain”, I looked forward to reawakening my grant reviewer skills to objectively identify the strengths and weaknesses of the document with the hope it would help pain patients. Unfortunately, I found it near impossible and beyond frustrating to review this document in an objective manner. The guideline is not organized like a typical guideline or tool kit. It is nothing more than a literature review of the harms and risks of opioids times 100. It is a warning for all doctors to not treat pain! Reading this document left me scared—really scared. It left me wondering what happened to the United States and to the rights of chronic pain patients? How could this be? No consumer groups or chronic pain patients were included in their peer review or “experts” process.
Yes, there are harms and risks with opioids, but a document meant to help primary care doctors in prescribing should be just that. It is biased in that it quotes very little about the realities of opioid treatment—that it is sometimes the only treatment modality left for some people. Even the DEA and 21 Health Organizations wrote, “Promoting pain relief and preventing abuse of pain medications: A critical balancing act” which states “Effective pain management is an integral and important aspect of quality medical care, and pain should be treated aggressively… Preventing drug abuse is an important societal goal, but it should not hinder patients’ ability to receive the care they need and deserve”.
The guideline talks about other medications and treatments yet fails miserably at discussing the lengthy side effects and risks of these treatments. They are conveniently omitted. The statistics in the Background section do not delineate criminal activity from actual chronic pain patients in a pain management type setting nor does it flesh out overdoses or drug use that involved polydrug use of illicit drugs or alcohol. Instead of a literature review detailing harms and risks doctors need supportive information. I would hope that a doctor knows the risks of any medication they are prescribing.
What Pain Management Guidelines Should Address
The guideline should explain that primary care doctors may be the only opioid prescriber in a patient’s area as most pain management doctors no longer manage chronic pain with opioids and specialists refuse to prescribe. Primary care doctors have by default become pain management doctors. As such, pain patients should not be punished for this trend. Also, doctors need to learn how to educate patients on the difference between physical dependence, tolerance, and addiction/misuse of opioid medications. Just because you are on pain medication does not mean you are a drug user or an active addict.
Patients need to be taught basic opioid safety—keeping the opioids locked away and out of teenagers’ hands. Many patients are naïve to think their teens would never consider experimenting with their meds or visitors won’t snoop through a medicine cabinet. Providing real-world information will prevent unnecessary overdoses NOT limiting chronic pain patients their pain medication.
The CDC is clearly not the appropriate agency to spearhead opioid prescribing guidelines. They are good at authoring literature reviews on ebola and trying to find cures for diseases. They are NOT equipped to publish guidelines of this manner. This is not an epidemic as the media is reporting. Overdoses and drug abuse are rare in the chronic pain patient population. There is no evidence chronic pain patients become heroin addicts. In fact, the only heroin addicts I’ve met who used to be chronic pain patients were those who were cut off from their doctors with no treatment plan. Proper pain management actually prevents illicit drug abuse. Hopefully the chronic pain patient’s story will be heard. So far, the government and media have turned a blind eye to them.
Photo by danilo.alvesd on Unsplash.













my wife passed away in 2016 from acute pancreatitis. I live in a Cincinnati Ohio Suburb and I can tell you its the same bs here too. Theyn never helped her 1 time oh wait yes they did they helped her become a pill seeker on the streets. I would go find her some myself. That woman was in pain just like you all are saying. You will do anything to get out of that pain. Unfortunately for me I had back surgery and was on opiates. She would take then from me and I would go without BC she was my life. So I get her in pain management. Now I am sure people on her know the difference between percocet and vicodin. For that pain vicodin just isn’t going to cut it, especially 5’s. That is ask they sighs give so needless to say she was thrown out for have p having percocet in system. Its not bc you are a junkie its bc that woman was in so much pain. I was about thrown in jail for laying hands on her Dr. It changes peoples lives for ever. She weighed 110 pounds soaking wet and was a looker. Man was she.. Her Belly swelled up so big she weighed 160 pounds. They never did anything for her no procedures of any kind no meds BC no one would see her after getting booted out of PM. She was 52 when she died and for 5 years she wished she was dead. My life shattered before my eyes left with so much anger, to me they need sued and everyone effected be by this get to stand before them and being able to tell them what they think and what should be done to those that swore to help the sick not bend the knee to these Idiots in control. They are idiots. Come see me big pharma Biden Secrete service wimps. I really don’t Care 6 years without her and I’m still lost
Thank you for this platform for those of us suffering miserably and endlessly, and in my professional and personal opinion, absolutely unnecessarily! I was a RN for nearly two decades before sustaining a serious work related injury resulting in 5 herniated discs and completely trashed knees requiring more surgeries than you can even imagine! (15, and we’re not done yet).
I, very unfortunately was exposed to a negligent surgeon who attempted to perform a Lap Chole on me to remove my gallbladder, under very urgent conditions, but the outrageously evil hospital in our town, (and the only hospital at that time) failed to inform me that the surgeon had 26 pending lawsuits against him, and the majority of them were for lap chole’s he’d messed up on! Clearly he was NOT qualified to perform surgery, but I didn’t find this out until after the tremendous damage was already done! (He’s now in Montana harming more patients) ???
After my Lap Chole, It first started out with SOD, Sphincter of Oddi Dysfunction, which I promptly sought treatment for, only to be told that there was not one single provider, nor place in my State that provided this type of treatment, and yet, the GI clinics in our state advertised themselves as “Cutting Edge.” Please!!!
Every time I’d get an attack an seek help, I’d was treated like I was a hypochondriac, or some crazed med seeker! What a friggin joke! All I wanted was too get out of pain, get well, and get my life back! The ER “Doctors” would outright refuse to do the tests and CT Scans requested in writing by my PCP, and I was basically refused treatment! (One idiot ER doc with his God complex, rudely informed me that I do NOT have pancreatitis and refused to do the CT Scan). Man was he ever a moron, cause I had a more accurate test somewhere else, showing just how serious my situation was. So even though I have just continued to get sicker and sicker, I DO NOT TRUST DOCTORS, NOR DO I GO TO THE E.R. ANYMORE! I avoid them all like the plague.
I have since been diagnosed with not only chronic pancreatitis, but EPI, which is Exocrine Pancreatic Insufficiency! This is very serious. VERY SERIOUS. My pancreas has atrophied, and will continue to do so, (and often leads to Pancreatic Cancer) ? and I can’t take any of the suggested Enzymes because of the SOD, so when I take any enzymes I almost immediately have an outrageous attack that takes me out for several days or more!
The Antiemetic/anti nausea meds that the lousy insurance company will only pay for is NOT conducive to my surgical history, nor too some of my current health issues, directly related to the Pancreatitis. I need the injectable, and being a RN, there should be absolutely ZERO problem with them providing that for me, but they give the most ridiculous excuses ever! I truly believe it all comes down to the might green greed myself! But the meds they’re giving me are just continuing to cause more problems! I loath insurance companies!
I have so many horrible, miserable, excruciating painful health problems that I haven’t been able to leave my house in over 18 months, and now I just recently found out the state board of pharmacy scumbags wants to lower my meds once again! I have taken it upon myself to lower my dose a few times, without their “prompting” threats or anything, because the meds just aren’t good for you long term, but when you really need them , you need them! I’ve never ever had any issues with these meds, and absolutely no problems cutting down, but I can’t take any NSAIDS, due too a SEVERE allergy resulting in an overwhelming amount of systemic edema, heart palpitations, itching, etc etc! I end up looking twice the size of the Goodyear blimp! It’s awful!
I’ve tried acupuncture, massage, kinesiology, relaxation techniques, meditation, natural medicine, etc etc etc!ive tried just about everything! Now I have no more money, lousy insurance, ZERO energy, zero trust, minimal hope, no help from anyone, cuz you really find out who really cares about you when your chronically sick! ???? and in my case it’s been the people I gave up my time, energy, and everything too help for many years! Happily I might add, and I’m not sorry I did! Even though they’ve all disappeared, I wish them well and pray for them all. Truly!
So here I am with chronic pancreatitis, a shredded rotator cuff and neck problems, two completely thrashed knees, and one which is basically only held together by skin, all the herniated discs, fibro, migraines, …..the list is too long, and there’s NO HELP, which means NO HOPE!!! I have no idea what to do except try to find a way to move out of this state to a place with actual, intentional, reasonable, effective, healthcare and healthcare providers! Is there even such a place? I don’t know, but I certainly hope so!
My sincerest apologies for sounding sour! Certainly not my intent. It’s been a challenging day actually, more so than usual, but again, thank you for this platform and for any and everyone out there, if you find yourself which the diagnosis of SOD, Sphincter of Oddi Dysfunction, PLEASE research, find and get to the right physician or whomever to get help as early as possible! Please don’t let yourself get to the point where I am, or you’ll be ever so sorry! And fo your very best to get the most comprehensive, yet affordable of course health insurance.
Best wishes too each and every one of you and I pray you all find the help you need and truly obtain good health again! People with good health should never take it for granted! It is a true gift and blessing Take Care and Be well!
I too have pancreatitis. I have had it since 1989 after my son was born. When I have to go to the emergency room my husband brings me and it always depends on who’s the own call Dr when I go. I never know what kind of treatment I’m going to receive because different doctors different treatment. Different staff different treatment. I have gone in plenty of times and had Pleasant experiences my pain was taken serious and they gave me Demerol IV relief and liquids. Then there are times when I’ve seen and if my amylase and lipase are not high they will send me home even though I’m in pain. I have pain meds at home I take methadone which is a drug that no doctors in Louisiana wants to prescribe so I’ve had to change Physicians 6 X since I moved to Louisiana because my doctors either do not take my insurance or they decide they do not want to prescribe the medication anymore. It’s very frustrating having to look for a doctor over and over again to prescribe methadone. The doctors here have no problem prescribing Oxycontin which is stronger than methadone. Most of the time when I go to the hospital or the ER I have to fight to be seen. When you’re in excruciating pain the last thing you want to do is have to argue fuss and fight with the staff to get them to understand that you are in severe pain that you have pancreatitis and that your meds at home or not strong enough. I have been medicated at the ER and sent home with no meds because I have meds at home after explaining to them that my meds at home aren’t working because they’re not strong enough but they will not admit me to the hospital because my amylase and lipase are not in high numbers. what they don’t realize is that when you have pancreatitis as long as I’ve had it and I’ve had the Whipple surgery so I only have a piece of pancreas left sometimes your amylase and lipase does not Elevate until the next day. I’ve had that happen to me once I went to the ER and the ER doctor was going to send me home and I told him that I could not go home because I was in severe pain and that my meds at home or not working and he argued with me saying that there was no reason for him to keep me that he had to have a reason for me to stay and I told him the reason to stay was that I was in severe pain and he said that they had to have something that they could put on the paperwork to justify them keep him in the hospital. After arguing with this doctor for what seems like an hour he finally decided to hold me over night and send me home in the morning. Well surprise surprise by the time they came to draw my blood that morning my amylase and lipase was through the roof to say the least this doctor walks into my room in the morning and tells me ma’am your amylase and your lipase is elevated and offered no apology for for the trouble he caused the night before. I’ve been to almost every hospital in my town we have for hospitals and I’ve been to all four simply each one that I go to I’ve been treated badly so I just go to another hospital so now I’ve been to all of them and I just pick and choose which one I’m going to try each time I have an episode because no matter which hospital I go to I never know what’s going to happen. I’ve been longing to find a pancreatitis group that I could possibly join to find out more information on pancreatitis and what the outcome is because my doctors aren’t telling me anything. I only have a piece of my pancreas left and I’m often wondering am I going to die from pancreatitis is it going to turn into cancer I have several other issues going on and I think they’re from my pancreas not performing the way it should but the doctors that I have seen or not doing the correct test or not doing what needs to be done to find out why I’m having all the other issues I’m having too many to name but just strange feelings in my body I have more bad days and good day’s most times I’m stuck in bed and the few times that I am able to get up and get around I’m still not feeling all that well but I do what I can do my prayers are with all of you and I pray that we find a solution to our problems. If anyone knows of a pancreatitis group I can join please let me know thank you to you all and may God bless all of us.
The author was against pain medication for CP. Until she got it herself.
Everyone else is the same way. It isn’t them, so who cares?
If the author hadn’t gotten this incredibly painful disease, she would still be advocating anti-opioids to keep them out of the hands of teens.
Instead of the opposite, think about that.
No one cares unless it affects them, & then they are in too much pain to advocate for themselves, not that it makes a difference anymore.
FYI, the profession most likely to abuse narcotics is…..Drs & the medical profession. Do No Harm no longer matters. Although every gov agency DEA, FDA, CDC, and Drs, media, & politicians are to blame ….Drs can’t do their job for fear of the DEA & losing their licence. The DEA gets paid per bust on Dr, giving them incentive to crack down on legit Drs. The VA has cut meds to Vets by 70% or more, causing suicides to soar.
The only logical conclusion to this witch hunt (harm reduction is illegal for addicts) is that the gov WANTS CPP’s to die of pain, suicide, or illegal drug use. They WANT the NON- EPIDEMIC problem of opioid OD’s to continue to kill addicts, or harm reduction would be legal. They would take CPP’s, Drs, & recent AMA DID stand up to politicians passing blanket laws telling them how to treat patients, in a unprecedented move.
CDC states polydrug use, suicides, & downright lies by the media of 100’s of people dying a day by PRESCRIPTION PAIN MEDS. A blatant LIE. OD’s aren’t in the top ten leading causes of deaths according to the CDC, but media reports it’s the 2nd leading cause of death. Suicide IS in the top 10 & rising.
The only way ALL these people would be on the same page is greed & an AGENDA!
And after thinking they MUST be killing us on purpose for years, I came across….Agenda 21 which states the growing population is a threat to the ability for the Earth to sustain itself. The G8 Countries met in RIO in 1993 for the UN Summit & decided they would reduce the population by 2/3 by 2050. The US is reported in the lead.
But how? How are they reducing the population? Having people kill themselves over pain & OD’s would be a good start…..2 undesirable populations, the disabled & poor who are on disability, medicaid, i.e. government programs. It’s a win-win for them. It’s not like they’re hiding the goal to reduce the population, it’s in widely available gov documents (wikipedia a start).
They count on people not reading it.
The DSM-5 (Drs and INSURANCE CO’s BIBLE) was updated, now “addiction” is the same as “physical dependence”.
A 80 yr old dying of cancer is EXACTLY the same as a 25 yr old recreational drug user at a party! Why? The Dr who headed the revision also works for a Big Pharma Co developing…..a new addiction drug! For EVERY kind of addiction! Now insurance co’s will pay for her drug. She was asked if she thought it a conflict of interest, she said “No, they want the best researchers & the best working on the DSM revision”. One Dr. Stormed out (it was reported) for not being on board with some of the changes.
I’m sorry I don’t have the link, I’m sure it can be found under “DSM-5 revision”.
Why aren’t the 150 MILLION CPP’s being given a voice?
Suicide is the only way to go.
A Las Vegas station did a week-long series on the abuse of pain pts. Kim McKim has some good videos “The Slow Death of Compassion for the Chronically ill”. On YT.
Dr. Forrest Tennant is working into his 80’s because his pts have no where else to go. He’s been the leading force on chronic pain for decades. He has many alternative treatments, but refuses to cut back his pts pain meds when he deems it necessary to their health. He’s been very vocal. He also has a Handbook for Chronic Pain online.
Good luck to you all, it’s a quagmire. And very well researched article……rare these days.
Sounds familiar. I have been treated in hospital for 4 years for chronic pancreatitis. They gave me dilaudid and fluids. Last week I had an episode and they refused to treat me. Hospitalist says I really wasn’t in that much pain. She was sure I am drug seeking. Sent me home with no relief. I found I could manage pain at home with combination of Percocet and advil. Now no one will prescribe the Percocet. People wonder why drugs are bought on the street.
Brook, I couldn’t have said it any better. I’m getting injections, blocks and am on a dose that leaves me up every other night suffering in agony. I was told by my pain management doctor that he needs me to cut back on my dose again. I am so scared as to how I will cope, and how this is going to affect my ability to raise funding for my islet transplant hopes. I even consulted with transplant surgeon to please just take my pancreas from me. He said no because I am still a good canidate. We lost ourlocal pancreas clinic after Obama care took affect. No sick ones allowed. I wish they understood the severity. I researched and found a study that suggested the narcotic recommendations for CP were not sufficient. It said the dose should be increased for those suffering sith CP. I am not an addict, nor an alcoholic. My CP came on from chemo meds given to me for RA. I appreciate your letter, and advocacy in this matter. I have an online support group, and am friends sith many who are suffering the same fate. So far this year a seven year old boy died in an Er from a doctor who sent him away four times that day. They just let him die. Then came the lawyers and we we were told it wouldn’t make news because of litigations. Then a member of another group decided to end his life live via Skype while other members were trying to save him. That left a stain in my mind. I think he thought it might bring some much needed awareness. And now after CDC guidelines and so many losing access to treatment or pain relief. It’s suicide or some are just dying from complications, and one lady was totally misdiagnosed and had pancreatic cancer no CP. I became a support for her but I felt do lost as to how to keep my hopes up and quiet my own internal fears of cancer coming before trandplant. Now that the new studies prove that we will eventually have it progress to pancreatic cancer. It still is a disease full of stigma and judgements, and not well understood. I’m not sure how many lives it’s gonna take for the powers that be to give some mercy and trust to us who are plagued by an organ dying inside us? 🙁
I am so sorry to read your doctors want you to keep reducing your medication. Pancreatic pain is awful and tortuous. Unfortunately everything you said is true. CP patients are treated like drug seekers and no compassion or sense of urgency. Hopefully through our patient voices and advocacy this will change. I wish you the best.
This topic boils my blood!!!! My husband has CP (he was diagnosed 4 years ago) with plenty of hospital visits n lots of miss treatment (as well as some good).
Every time he would get a flair up i would start to feel sick of my stomach, just thinking about who we will run into in the hospital (good staff or a bad one)!!! I have cried I have been mad, but NOW I fight back!!!!!
I take all his medical records with me n I challenge the Dr.!!!! The last visit my husband had on Dec 25th 2017 the Dr was so racist n rude that I complained n I will not stop complaining till something gets done in his local hospital!!!
I told them that “I live here n this is my local hospital n as long as we live here we will continue to come here for help!!!!
I will say we do have an awesome PCP that will give him pain meds if admitted also his old pain Dr does rounds in our hospital, so if he needs something stronger or changed she will do it. As well, we just got a new pain Dr (My husband has a pain pump for about a year in February, not yet fully adjusted) our old pain Dr said he is aggressive in treatment!!!
What I have gathered with this illness is that u have to find a team a team of DR that understand you as a person n patient with a chronic illness. I constantly try to show my part in this (going to specialist, having the proper Dr’s n care in place) but when all my efforts to show that we r responsible in his care n we r not drug seeker d ont work I go to my baddle mode!!!!
I question the Dr oath to help people n the fact that they vowed to ask there colleagues for help if they don’t understand his illness, also I will complain to the highest person available (always remaining professional) I will talk to patient advocate and most importantly I WILL NOT GIVE UP ON HELPING MY HUSBAND GET THE TREATMENT HE DESERVES!!!!
We can’t let the health care profession to dictate our care we r the sufferers n only we know what we need for care, not a healthy person reading textbooks about a matter then all of a sudden they r an expert on what we the suffers, the family’s r going through with this illness!!!!
I can’t tell u the last time I had a plan or a trip?!?! Y??? Cause I’m scared to leave my husband alone!!! Scared that if I’m gone they will KILL my husban…. a father, son, and a brother to someone!!!! Is this what we have come to? A life on opioid is not worth saving? I have never been so disgusted by the health care profession like I am now!!!!
I hope n pray that together we will get hospitals to have a proper protocol for a diagnosed CP/P (or any chronic illnes for that matter)sufferer. Best wishes to all n God bless!!!
Thank you for this article and great insight and information. Although I do not share your medical issues, I understand your pain and frustration. I have two very rare progressive “syndromes”. I am also a recovering alcoholic who had to make the same decision to take pain medication. They are medication not drugs. There is a big difference. I drank as a way to self medicate because I was desperate for pain relief and acceptance. My family who has never accepted me has accused me of seeking drugs. They have never even asked me about my conditions or offered to help me in any way. They don’t get the right to make such accusations. They do not know or care to know that I have NEVER abused or misused my pain MEDICATION. I need this medication to much to ever risk losing it. It took my almost successful suicide attempt before any doctor ever believed that the pain was unbearable and never ending. That’s the problem with having conditions so rare that most doctors have never even heard of them before. I’ve had many doctors call me a liar when I tried to explain my conditions. It has been almost 30 yrs since I was diagnosed correctly and yet nothing has changed. If doctors don’t even know or have a clue about my syndromes and all the associated problems, how can some bureaucrat make informed decisions about whether or not I and others like me need these kinds of medications? I already have enough problems with Medicare denying things I need because my conditions aren’t included on their lists of acceptable diagnosis needed for their approval. It’s just ludicrous that some pencil pushers with unacceptable opinions get to write policies, make unfair uneducated assumptions, and deny coverage for people and conditions they know nothing about. They need to quit listening to the uninformed public hype. Maybe they could just sit down and really listen to those of us who suffer the pain. Listen to the degradation and pain we go through every day of our lives. Listen to those who are still waiting desperately for someone to acknowledge their pain and help them. Don’t make our lives any harder than it already is. Don’t make us fight for our lives. Don’t make us use the little strength and energy we have left on fighting an unfair system. We need to use that energy on surviving not fighting. I should apologize for this being such a long message, but I won’t. I am fighting for my life and the lives of people like me who live with unbearable pain. I will never apoligize for that.
I have had “autoimmune pancreatitis ” since the late 1990s. Never drank, never did any drugs. The pancreatitis started after having a TAH. I do think it has something to do with hormonal imbalance. I also have a blood clotting disorder and could not take hormone replacement. The first three years of this disease I was given Demerol IV, a drug they don’t even use any more because it was in safe. For 10 yrs went to pain clinics. All they did is.write u a script and go to the next patient. When I decided I had enough of all the prejudices of health care workers for people who really need it, I called the pain clinic and said ” I would like to be weaned down to the lowest to level possible. They replied “we do not do detox”. I was appalled. I thought the whole goal of pain management is to have the patient who has a very well documented painful disease, I knew I could not function without any medicine but I thought the whole idea of a pain clinic was to help the patient with pain to be able to be on the most optimum pain medicine to be as independent as possible and be able to function in their active activities of daily living. So now I still continue to be hospitalized monthly for acute flare of pancreatitis, pain doctors now only will do nerve blocks, which I am not a canidate for because of my history of blood clots. NSAIDS I can not take because I am on blood thinners, so for the past 22 yrs. the only thing that has been able to control my chronic pancreatitis is opiates. I set goals with my doctor, both short term and long term. I have built up a tolerance, but I do not get a “high” feeling. I get the feeling of thank God I can get out of bed, get a shower and do my activities of daily living without lying in a fetal position in pain. In bed, which would eventually end up in the hospital. I am appalled by the judgement of health care workers that go along with patients that use chronic opiate therapy for pain. I have told many of nurses, doctors, ect. “Until you have walked a mile in my shoes, than u can judge.” So there are so many cases with patients like me, that are not black and white. Their are many gray areas and many patients like myself that need opiate therapy in order to function. The FDA needs to look at patient is ta on a case by case basis. You either fit in the black and white catagory or you need to look at the thousands of people in the gray area in which these drugs just can’t be stopped. It needs to be documented what medications that patient has tried or in my case the many non opiates that can’t be taken because but are not able to take because of allergies or because of their past medical history. If you take away the doctors right to adaquately treat their patients and the includes being able to prescribe opiates than I believe their will be a rise of those patients who need opiate pain meds trying to obtain them illegally. I think their will be an even higher rate of crime, as well as overdoses. Thank you for allowing me to Exspress my opinion. Tracy Finke
you are wright been there my story is almost the same now its turned to cancer because of them yes them doctors hospitals and staff they thouhht i was a junky even after being in the hospital 11 times in 2 years did they think i was liking that, some times weeks at a time. so i gave up on them and suffered with the meds they gave me some times wishing i was dead now it s over well bed to couch was not any fun so good luck and god bless.i do not care about me but my family payed and still are.now they get it the hospital and staff to late for sorrys wait it will happen to them not my wishes but how it works god bless…
Gary, are you getting any better treatment, especially since having your pancreatitis now turn to cancer? I hope your still kicking, and finding options for care. I will be creating a wall for people who are dying from this disease. I want us to leave our names as the martyrs we’ve bevome, so that the medical community can contemplate the true cost, and remember.
I have porphyria, acute intermittent. It’s a somewhat rare blood disorder, so rare that, if hospitalized somewhere where my Hematologist does not have privileges, it is almost always misdiagnosed. Pancreatitis is usually one of the first guesses, which leads me to believe that our pain is similar. As I’m sure you know, “A Couple of Asprin” isn’t even touching this pain, and while I too hate the ‘Fog’ of any pain meds, this pain is enough to drive you insane, literally. Thanks, in part, to the drug seekers and dealers, and in part to the hard-hearted “healers” in the Emergency Room, and even the Pain Doctors we are referred to by our other physicians who are too lazy to research their new cases before they see the patient, WE have to suffer. I’ll never know what I did, or what ANY of us have done to live like this…..
Brooke, your article is so educating I wish everyone could read it. I will share and share!
Thank you for putting your story to helpful words. I am saddened by what you have gone through and go through now.
I hope people will make comments on the CDC guidelines before it cuts off Jan. 13, and cite experiences like you have here. We need people like you to help us through these painful and frustrating journeys.