Between 1962 and 1982, I was a pediatrician at Cleveland Clinic, a multispecialty medical institution. Because I was a consultant pediatrician. doctors in a private practice referred some of their more difficult patients. I was confronted with a number of children who were experiencing emotional diseases such as Attention Deficit Disorder (ADD), Learning Disability, and Hyperactivity. The usual explanation for this kind of emotional disease is poor parenting. Therefore, I would sit down with the parents and discuss their approach. In most cases, it was healthy, but when I looked into the diet of the affected children, I found that in each and every case, it was full of empty calories, particularly from consumption of sugar and fat, consumed for their sense of taste. Indeed, this consumption was actively encouraged, since it provided the child with obvious pleasure.
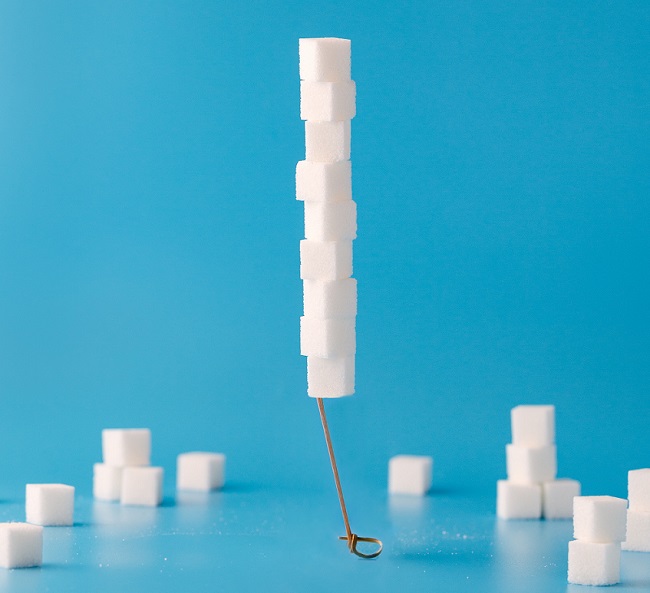
Sugar Induced Cellular Energy Deficiency
I turned to the library and read the details concerning the processing of sugar and fat in the body. Without going into the details, vitamin B1 (thiamine) stands at the head of the complex machinery that enables our cells to turn food into energy. I concluded that cellular energy deficiency in the brain was causing distortion of normal brain function in these children, I looked into what research was available and I found a 1935 publication by Sir Rudolph Peters, a famous researcher who worked at Cambridge University. He was trying to discover the role of vitamin B1 (thiamine) in the body. It had only recently been discovered that dietary thiamine deficiency was the cause of beriberi.
It had also been found that thiamine deficiency-induced in pigeons produced the histopathology that had been observed in humans with beriberi. He was therefore able to study the action of thiamine by creating what is known as a brei, a preparation of brain cells taken while the pigeon was alive. He then placed it under a microscope. The cellular activity, known as respiration, could be studied. He made a similar preparation from the brain of a thiamine replete pigeon and placed the two together under a microscope. There was no difference in respiration between the thiamine deficient cells compared with those that were thiamine sufficient until glucose was added to the preparation. The thiamine sufficient cells immediately began to respire, whereas the thiamine deficient cells remained inactive. This showed that glucose was the main fuel for brain cells and that thiamine was necessary for its consumption. He called this the catatorulin effect. Not only this, but Peters found that the deficiency was more severe in the cells from the lower part of the thiamine deficient pigeon brain, providing an important clue. We now know that the lower part of the human brain is peculiarly sensitive to thiamine deficiency. This research was extremely important because it formed a foundation that led to understanding oxidative metabolism.
The high sugar diet was affecting the brains of these children and I found that supplementing them with thiamine made their emotional symptoms disappear. I was in fact imitating the catatorulin effect. I found this very intriguing and began library research on the biological role of thiamine that has continued to the present day.
Thiamine Is the Spark
Without going into details, it stands at the entry of glucose into the complex cellular machinery that produces the energy required for all the functions of the body. Much of our food is turned into glucose in the body and acts as cellular fuel, particularly in the brain. Oxidative metabolism, to put it simply, is the combustion of glucose. Combustion in the body is known as oxidation and although the analogy is too simple. Thiamine provides the spark like a spark plug in a car that ignites the gasoline.
If glucose provides fuel for the brain, the children with emotional disease were getting plenty of fuel, so how could I explain this excess as the cause? We have to turn to analogy. Some older people will remember that the early cars all possessed a choke mechanism that introduced a rich gasoline mixture to start a cold engine. But if the choke was not removed when the engine was warm, black smoke came out of the exhaust pipe and the engine ran poorly, indicating poor combustion and energy production. A similar thing happens in the body, particularly in the brain. An excess of fuel overwhelms the ability of cells to combine it with oxygen like a persistent choke. The result is that the brain cells work inefficiently, giving rise to changes in behavior. It made the administration of thiamine quite rational.
Using a vitamin for treatment was not even suggested at that time. I took early retirement and joined a private practice that specialized in nutrient treatment. This was an early example of what has come to be known as Orthomolecular Medicine, which involves the ingestion of molecules that are well recognized by the body.
Behavior is a function of the brain and whether it be purely mental, or gives rise to bodily activity, requires energy. Psychosomatic disease is not due to the patient’s imagination. It is the result of a declining ability to produce sufficient ATP. This leads to the obvious suggestion that disease is a variable manifestation of energy deficiency dependent on the severity of the deficiency and its cellular distribution.
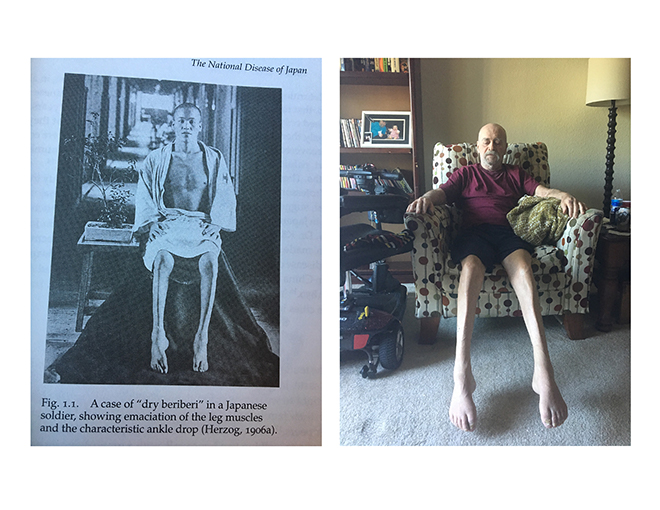
Thiamine Deficiency and Dysautonomia
One of the important results of thiamine deficiency is dysautonomia, dysfunction of the autonomic nervous system. This is the nervous system by which body organs are controlled by the lower brain. The deficiency is rarely seen as a cause of disease in America so the symptoms are attributed to other “more acceptable” conditions. Usually neglected, sometimes for years, thiamine has to be given to the patient in mega-doses to restore normal function. Damage to the affected cells may cause poor or no response. The research on beriberi, exclusively performed in China and Japan, discovered that recovery was most likely when the blood sugar was normal. If it were high, recovery was slower and if it were low, recovery may not occur at all. The dose of thiamine had to be huge to cure a patient of long-standing beriberi after its deficiency had been found as the cause of a widespread disease that had occurred for thousands of years.
Prevalent in rice-consuming countries, if and when the peasants made more money, they would take the rice to a mill where the cusps were removed. They would then serve the white rice in a silver bowl and invite their friends to demonstrate their newly acquired affluence. Of course, they did not know that the vitamins were in the cusp around the grain.
Thiamine Dosing Varies
I had found, ironically enough, that my insomnia was caused by thiamine deficiency and my diet has been supplemented with it for years. Being an entirely new treatment, it requires some detailed research, but self-research is time-honored. So I am going to describe a recent experience that illustrates how thiamine affected my autonomic nervous system. I had noted that when I ate virtually any food at all, my nose would run. One day I was eating some canned pears and I experienced a rather severe choking fit and my nose ran like a faucet. I was taking 300 mg of Lipothiamine (thiamine tetrahydrofurfuryl disulfide) and 200 mg of a magnesium salt. I concluded that the dose of TTFD was too great and lacking in balance with magnesium, which I increased to 400 mg. I reduced the dose of TTFD to 250 mg. Even within days, there was an improvement. The pharynx, esophagus, and nostrils are controlled by the ANS and the dose change was born out of my unique clinical and biochemical experience. Although orthomolecular medicine is in its infancy, it is hoped that it will become the orthodox medicine of the future. Not only is it non-toxic, but it is also extremely efficient and I have helped thousands over my 61 years of practice.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.










Tall your doctor to read my posts on HM.
You have classic beriberi and it is probably a combination of genes and diet. You complain about your health while causing it. You have to stop eating “junk” foods and escalate the thiamine dose slowly to try to find the “ideal dose” for you. It has no toxicity. The thiamine should be solitary until then when you can add magnesium, B complex and a multivitamin.
Dr. Lonsdale,
I just want to say Thank You!! Your work and the wisdom you share from your decades of experience and knowledge have changed my life and the life of my family.
Every new article you submit here on this site I read and take notes; I even have a Note saved on my phone “Dr. Lonsdale says:” where I keep highlights from your articles including a Boolean notation. This week I will add a couple of notes; one on blood sugar level not high OR low (I struggle with hypoglycemia). Plus, I have also had the nose running like a faucet so will keep in mind working on Magnesium/Thiamin balance.
Thank you, again, for sharing your insights. Even while retired, you are still helping people regain their lives!
Hey Dr. Lonsdale, I talked to you almost a week ago on here and you responded to me and suggested Lipothiamine. I then wrote you a reply but you didn’t answer me. I sent you the same reply two times, but on the second reply I added additional information and questions for you. The one I would like a response to is the one I posted on May 19, 2022 at 7:36 AM and it’s on the page of your other article “IT ALL COMES DOWN TO ENERGY”.
******P.S. can a paradoxical reaction also include worsening depression and emotional problems (which I already suffer with)?.
Hi,
Dr. Lonsdale is 98 years old and volunteers to share his knowledge when he can.
Ok I understand. Yeah I’m not having any luck so far with my thiamine treatment and I’m very disappointed and frustrated. I actually wrote to you (for the first time) on the other article you yourself posted a few days ago. Maybe you can read my convo with Dr. Lonsdale on the article he posted (“IT ALL COMES DOWN TO ENERGY”) and any advice you can give me be greatly appreciated. Thank you.
P.S. I bought your book yesterday and it should be arriving tomorrow.
Again, consider writing up your entire case for a post. That way, we have all of the details in one place. It is near impossible to tell what is going on without that.
*********Hi Dr. Marrs, so this is the entire thing you asked for from me, sorry I took several days to get back to you. This is my convo with Dr. Lonsdale and I went back and edited it and added some more stuff.
Hello Dr. Lonsdale. I’ve never spoken to you before, but I really need your help and advice. I found out about you, Dr. Marrs, and Elliot Overton while I was online while reading about dysautonomia. I haven’t read your Dysautonomia & Thiamine book from 2017 yet, but I’ve been reading up as much as I can online about you and by reading alot of articles on this website, watching a bunch of Elliot’s YouTube videos, reading posts and blogs on Reddit, and also by joining the “Understanding Mitchochondrial Nutrients” group on Facebook. I’ve been suffering with about 30+ symptoms ranging from 24/7 lightheadedness/dizziness, slight blurry vision, light sensitivity, noise sensitivity, severe depression, extreme panic and anxiety feelings (impending doom), constant adrenaline surges, body tremors where my hands always shake and my body vibrates with these buzzing sensations, heart palpitations, chronic constipation (since I was young), sensitive stomach and always bloated and gassy, temperature regulations issues with always being hot and sweating and then my feet and hands get cold, shortness of breath while at rest or with any exertion, SEVERE debilitating fatigue, terrible insomnia that even sleep medication can’t completely help, trouble swallowing, feeling both full and hungry at the same time and feeling like food is just sitting in my stomach and not being digested properly, increased heart rate and palpitations whenever I eat or swallow something (even water), brain fog, short and long term memory issues, hard-to-manage sugar cravings, joint pain and joint stiffness, body pain, body weakness, muscle pain and cramps, numbness and tingling in extremities, feel like I have the flu all the time, urinary incontinence (for several minutes each and everytime, but only after I urinate), plus some other symptoms that I can’t remember at the moment. I am a 35 y/o male and I have literally seen and been tested by over 20+ doctors since 2014. I have seen almost every specialist there is and have pretty much ruled out almost all other medical conditions that could be causing my symptoms. But this is what I have been diagnosed with and what I DO have:
1) Ezcema (Since my teenage years)
2) Dry Eyes (Since my teenage years or early 20’s)
3) Hemochromatosis (carrier) -diagnosed in 2020
4) MTHFR gene mutation (found this out in 2015)
5) GERD (within past 2 years or so)
6) small Hiatal Hernia (found within past 3 months after having an Upper Endoscopy w/ biopsy)
7) Small Fiber Neuropathy (did a nerve biopsy in 2021)
8) Autoimmune-related arthritis (seems to be possibly Psoriatic or Rheumatoid, but my Rheumatologist is not 100% sure yet of which type). (I was diagnosed in 2021 after doing certain bloodwork and MRI’s of my hand and foot.
8) Dysautonomia (unknown which type exactly, but in June 2021 I did a bunch of autonomic testing with my FOURTH Neurologist and it confirmed this).
9) POTS – I have all the symptoms of POTS, but two Tilt Table tests were done and unfortunately my heart rate didn’t go high enough to qualify me for a POTS diagnosis, but the symptoms are still “identical” with my dysautonomia and I still believe I have it. And my current Neurologist even thinks I have it too.
10) Bipolar (Type 2) (diagnosed in 2019)
11) Severe Depression (since 14 y/o)
12) Severe Anxiety & Panic Attacks (since 14 y/o)
13) PTSD (for awhile)
14) Low Vitamin D (all the time). For some reason when I would take this in the past I would get increased anxiety, irritability, and heart palpitations while taking 2,000 IU (once a day). I don’t know why and I never used to take other vitamins besides my Vitamin D, but this always happened. I have a new bottle with 5,000 IU and I’m assuming because I wasn’t taking magnesium with it, this is why I was getting this reaction? Or it was maybe the fillers inside those products? That’s all I can think of. My new vitamin D brand doesn’t have any fillers in it.
*******It’s been FIVE weeks since I started thiamine (THIAMAX) supplementation and this is my current dosage (as of today) of Thiamax and all the other supplements that I started as well (along with the dates I started taking them).
1) THIAMAX (Thiamine TTFD) – 500 mg – once a day) – started on April 19, 2022
2) MAGNESIUM complex (this supplement contains Glycinate, Taurate, Orotate, & Malate) (300 mg – twice a day) – started on April 27, 2022. As of a few days ago I stopped taking that supplement containing 4 different types and started taking Magnesium Taurate only (200 mg – twice a day, but will eventually try 400 mg – twice a day when I can build up to it).
3) POTASSIUM CHLORIDE (297 mg – twice a day) – started May 2, 2022
When I first started taking the Potassium I started to feel crappy with mild stomach aches/discomfort, back pain and body pains and joint pains, and now I’m getting short of breath and it feels like my breathing is constricted and that makes me kind of nervous. The SOB is worse when I’m lying down or sitting down and it feels like I’m not getting enough air. Everything was going ok so far until I started the potassium, but MAYBE it’s the magnesium doing this instead? I already am short of breath all the time from my dysautonomia, but this feels different. And even when I started the magnesium (before starting the Potassium) I was getting more heart palpitations than I already do and my body vibrations and tremors (which I also already experience everyday) have become worse and I thought magnesium is supposed to stop these anyways? I’m so confused about that.
*******UPDATE: this has calmed down just a little bit, so I’m assuming it was my body’s reaction to taking magnesium and potassium?? It seems like each time I increase one supplement it depletes another one. But it still feels uncomfortable.
-should I be taking a supplement containing ONLY magnesium Taurate (this is what you suggest, Dr. Lonsdale). And if I’m deficient in magnesium, how much do you suggest I take each day? Because as of today I’m currently taking 400 MG total for the day and I still don’t feel any better and my palpitations haven’t gone away and my anxiety has actually increased.
– how do I stop this breathing issue? Is an imbalance of potassium, magnesium, sodium or calcium causing this? How do I fix it?
3) CALCIUM CITRATE 250 mg) – twice a day – started May 15, 2022
4) TRACE MINERALS supplement – I have it, but haven’t started it yet. It doesn’t contain Iron or Magnesium or phosphorus, but it contains almost every other important mineral. I bought it like that for a reason because I heard IRON is not good to take and I only want magnesium from one supplement instead of 2 and I only want Taurate because you recommend that version. Do I take a trace mineral supplement only once a day?
4) Vitamin E – 180 mg (how many times a day?). I bought it, but haven’t started it yet.
5) Vitamin C (timed- release version) – 1,000 mg (once a day?) I haven’t started it yet.
6) THIAVITE (B vitamin Complex) – Elliot Overton’s product. (I take one pill a day, but do I need a higher dosages of the B vitamins then I’m currently getting?). (Started on May 6, 2022)
******between the THIAMAX and the B-complex I feel pretty revved up and more anxious and jittery. I only tried taking B vitamins once before and my body couldn’t handle them. I finally realized (after reading online) that it seems that my body CANNOT tolerate “Methylated” vitamins. I think that’s what it is. I took a supplement with methylated B vitamins over a month ago and boy did I feel pretty sick and full of extreme panic. I took them for 6 days and I thought it was the paradoxical reaction, but then I read online that it was probably this reason and I’m under the assumption that my body would never adjust to these versions of the vitamins, so I bought non-methylated vitamins with no other fillers. So that’s what made me buy Elliot’s THIAVITE B-complex. But I’m still not feeling great on the THIAVITE anyways, but it pales in comparison to how god awful I felt on the Methylated B-Complex. Was that paradoxical reaction or is my body unable to (and NEVER will be able to) tolerate Methylated B vitamins. I have a MTHFR gene mutation, so I’m not sure which is the proper form of vitamins I should be taking. Thoughts?
7) VITAMIN A, D, and K (it’s a 3-in-one supplement). I started this almost one week ago and I seem to be tolerating this supplement ok right now (which is weird).
*****Vitamin D (5,000 IU), Vitamin A (900 mcg), and Vitamin K1(1,000 mcg) and K2 (1,800 mcg).
*******Do I definitely need to take a mineral/trace mineral supplement thought? If so, must it contain EVERY mineral? Even Iron? How important is this because online I’ve never really seen you Dr. Lonsdale tell patients they need to take this.
*******As I’ve already said I started the B Complex exactly THREE weeks ago and I started it about 17 days after I started the Thiamax because I didn’t want to start everything at once and then not know which supplement is causing which side effects. I’m usually very sensitive to most supplements and pharmaceutical medications and I’m shocked that I’m not really experiencing too much of a paradox (if that’s what this is because it’s hard to tell). Maybe I’m not deficient in thiamine or B vitamins? Although I have had a very poor diet and consumed a lot of sugar and fast food for several years. I’m not an alcoholic though, so that’s not an issue and I barely drink alcohol. And ever since I developed this dysautonomia I haven’t been able to tolerate alcohol or be able to enjoy a drink or two when I’m with my friends because it triggers my symptoms and makes me feel weird. I didn’t really have this problem a few years ago. Also I don’t use recreational drugs. But once again I feel kinda crappy again after taking B vitamins, but DEFINITELY NOT as terrible as the multivitamin I tried over one month ago including the methylated B vitamins. But it had ALOT of ingredients in in though. It had minerals, vitamins, probiotics, etc. That made me think that I was experiencing a paradoxical reaction. But anyways since starting everything else my skin has been flushed and I feel more hot, I’ve had an increase in anxiety and panic, an Increase in depression, and the joint pain and body pain that got a lot better with my arthritis medication I’ve been taking for the past year is now returning and I’m having muscle cramps.
*******Besides the vitamins I also take TRAZODONE (for insomnia), PASSIONFLOWER supplement (250- 750 mg a day – twice a day) for anxiety, and SULFASALAZINE (500 MG – twice a day) for my arthritis. Is the passionflower possibly interfering with my vitamin supplements? If I don’t take the passionflower then I really have nothing to help with my anxiety and it’s even more unbearable.
*******Dr. Lonsdale suggests for people to take a B complex AND a multivitamin as well, but isn’t that too much B vitamins between the both of them? Why do you suggest taking both? Instead of a multivitamin, I just bought all the vitamins separately (some of them). But I still feel that because of my battle with depression and anxiety, I might be the type of person who needs more B12 (for example). I’ve been on over 20 antidepressants and psych medications over the years and I don’t do well on them and they don’t do much for me anyways. And plus they are no good for you and I agree with you on pharmaceuticals being toxic for your body. I’d rather not be on any at all to be honest if doing the whole vitamins/minerals supplementation route ends up helping me instead.
But basically this is where I need your and Dr. Lonsdale’s help………..as I said I’m very surprised that my fatigue hasn’t improved on Thiamine and I’m on 500 mg of Thiamax right now at this moment. I started on 100 mg and I’ve worked my way up to 500. But NOTHING has improved. None of my neurological symptoms, nothing. And I see that that’s a good dose for most people. Some girl wrote about her POTS symptoms starting to reverse themselves after like 3 days and she was only taking 100 mg. What am I doing wrong here with my supplementation? I realize some of my 30+ symptoms are obviously from my neuropathy, arthritis, and psychiatric issues. But after feeling like I’m going crazy for years not knowing what the heck was going on with my body and my current neurologist testing me for autonomic dysfunction (which I pushed for by the way because I specifically searched for a neurologist who does this), I found out I have dysautonomia. But he said there’s not much to do for my symptoms besides going on medications (if I want to) for my symptoms. I don’t qualify for IVIG treatments to see if that would even work for me, so that’s not even an option right now. Living with dysautonomia has put me in an even deeper depression because if there’s nothing to reverse all my neurological symptoms and fix my nervous system, I will either get sick or stay the way I currently am. I’m 35 years old but I feel like I’m 90. I can’t tolerate exercise anymore and I used to be a gym person. I can’t do some of the things I used to do without having issues and symptoms and my whole quality of life has took a drastic turn. Besides my mental health issues (which have been very hard to treat as it is), I was a pretty physically healthy person about 3-5 years ago. I was on KLONOPIN for my severe anxiety and decided to come off it in 2019 after being on it for 5 years. It’s such a terrible drug and I came off it myself because I realized how bad of a drug Benzos are to be on. I made the hard decision to come off of it and It took me 8 months and It was complete HELL and I went through a tough withdrawal. But I had no backup drugs for anxiety. So I’ve been suffering ever since and I’m on Passionflower now, but it doesn’t so much at all. I actually thought that maybe coming off KLONOPIN actually caused my dysautonomia, but no doctor seems to know the answer to that. But all hell broke lose once I came off it. It must’ve been masking my dysautonomia because since 2019 I got a lot worse and developed all these weird symptoms that I finally can put a name on it. I now know I’m not crazy and that it’s my nervous system. But anyways……. I have so much fatigue that I can’t do even much without getting extremely tired, lightheaded, short of breath, and have these adrenaline surges and heart palpitations. The adrenaline surges are the WORST. I live in fear and constant dread 24/7 and even my therapist agrees with me that there’s a difference between having anxiety and having these adrenaline surges and that I should not be experiencing intense doom and panic 24/7. That’s because my nervous system is messed up and faulty. But I still work full-time and I’m amazed I still can (for now). I’m pushing myself, but I feel sick all the time and I call out of work ALOT. Most other jobs would’ve fired me by now. So I didn’t have any hope left until I stumbled upon you and your book and Dr. Lonsdale, Elliot Overton, and this whole Vitamin thiamine deficiency thing. But the point is I’ve been on thiamine (the best version – TTFD) for one month, I’m at 500 MG, I’m on magnesium and potassium, but yet I still have the heart palpitations. I thought this was the answer for me, but either I’m not at a high enough dose, or NOTHING is working because I’m not taking every single vitamin yet and none of the other minerals. I would like to point out that I’ve had extensive, very expensive genetic testing done and also had a muscle biopsy a few months ago and ruled out any Mitochondrial disease/disorder. That’s what my current Neurologist and Geneticist were both looking for. I’ve been worked up with alot of specific bloodwork and extensive testing by:
4 Neurologists, a Cardiologist, Rheumatologists, a Pulmonologist, a Vascular specialist, Dermatologists, my PCP, Hematologist, a Nephrologist/Oncologist, Gastroenterologists, Endocrinologists, a Geneticist, ENT specialists, an Orthopedist, a Chiropractor, Urologists, a Proctologist, a Neuromuscular specialist, an Allergist, an Ophthalmologist, and a Podiatrist. Some of these were just for other things, but almost everyone of these were to find out what was going on with me.
1) forget about me even being on 500 MG, is it possible that TTFD doesn’t work for everyone and I might need a different type of thiamine instead and then it might work? Not to mention that it’s very expensive to be on a high dose anyways because no matter what product I buy, that’s ALOT of pills and the bottles run out quick. I don’t care to spend it if this gives me back my life though.
2) what dosages of every vitamin (A, C, D, E, K, and B’s) and minerals (potassium, calcium, magnesium) should I been on and what is the maximum dosage I should strive to be at for all of them?
3) is it possible thiamine deficiency isn’t even the issue for me and it’s something else? Which I couldn’t even guess what that could be at this point. I’ve ruled out any cardiac or neurological conditions, respiratory conditions, etc. What do you think might be my problem here?
4) should I be taking any other supplements? Do I need huger dosages of certain B-vitamins or of anything else in order to improve my mental health?
5) do you or Dr. Lonsdale (even though he’s retired) do consultations over the phone. I live in New York. I really would love to be able to speak to you (if possible). I need help and advice. I really thought 500 mg would of done SOMETHING by now. I feel no better and I’m really worrying now and I’m very angry and disappointed to be honest because I thought this was the answer because if this isn’t it, no one knows how to really treat my dysautonomia. I’ve seen so many doctors because I’ve been so determined to find out what was going on with me and now I finally know…..DYSAUTONOMIA. Dr. Lonsdale replied back to this whole big message I sent and said that I have “Classic BeriBeri” and that I should stop everything I’m taking and then start on Lipothiamine (Cardiovascular Research) at 50 MG, wait for paradoxical reaction, and then start on Magnesium and a multivitamin. I wrote back to him. He never responded back to me after that. He never said to take a B-complex, what dosages I should be on for the Magnesium, and WHY I should be on Lipothiamine and if he’s had patients where TTFD doesn’t even work and other forms of B-1 do. I need to know this.
6) Elliot Overton told me on Facebook after I asked him why nothing has been working with the Thiamax so far that some people that have dysautonomia need a high dose of BIOTIN in order for the Thiamine to work. This is true because I’ve never read that anywhere yet? If so how much should I try?
*****I apologize for this being so long and that there are questions scattered all over the place, but I’d appreciate your response because I just want to get better and NO doctors have been able to treat me for this. And I don’t want to give up supplementation just yet in case I do have BeriBeri and maybe I’m one of those people who need a very high dosage of Thiamine (but I’m, not sure). Maybe I have absorption issues and the thiamine isn’t being absorbed. My diet is still poor right now. Anyways I wanted you and Dr. Lonsdale to have all the facts about me and my entire Medical HX, etc. I wouldn’t mind if you published my article on the website so that it can help other people. I don’t want to give out any personal info like my name though. What do you need from me regarding this? By the way thank you guys very much for all the work you do and bringing awareness to the medical field about this. You are helping so many people.
Hi, I have limited internet this weekend. Will review and get back to you on Tuesday.
You have classical beriberi and your sugar laced diet will prolong it
Hey Dr. Lonsdale how are you? I’m about to start intramuscular thiamine injections with my doctor and he’s gonna inject me with 100 MG once a week for a few weeks to see now I react and if I’m fine, he is ok with me injecting myself with it after that. He’s going to teach me how to do it. But you can tell he’s unsure about the dosage because thiamine injections is not something he deals with and doesn’t have much knowledge about. The entire injection (one month supply) will hold 30 ML and so technically if I wanted to, there’s enough in there for me to inject myself with 100 MG EVERYDAY for 30 days (since 1ML = 100 MG). I need to know if taking 100 MG (intramuscular) everyday is toxic and dangerous? And if I do this for the rest of my life will I cause neurological damage and mess my body up? None of my doctors know how to dose thiamine and have no knowledge about any of this. I feel that taking 100 MG once a week (intramuscular) is definitely NOT enough, but I don’t want to harm myself either. And also If I were able to receive a banana bag IV or a Myers cocktail I have to pay $200 each time because insurance won’t cover it, but I don’t feel that doing one of those once a month (which is what it would probably be) would give me enough thiamine to last anyways.
Yes