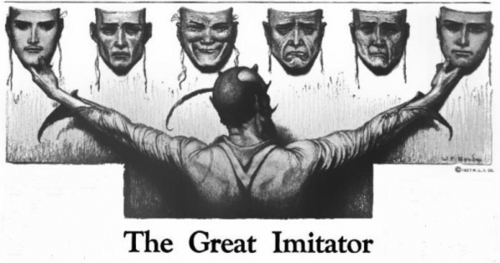
I wanted to share my experience going through thiamine paradox and my journey to heal. I am 27 year old girl from Italy and have been suffering from various health problems since I was 14 including a brain tumor that necessitated surgery, followed by Epstein Barr Virus, Hashimoto’s thyroiditis, multiple parasitic infections, antibiotic reactions, extreme and chronic fatigue, fibromyalgia, dysautonomia, SIBO, and gastroparesis. I have begun thiamine therapy six months ago and while some of my symptoms have improved, others have remained or worsened. I am not sure what to do next and am writing this in the hope that someone will have some answers.
Dysautonomia and Illnesses Post Brain Surgery
In 2008, I underwent neurosurgery to remove a benign tumor in my temporal lobe. It was very large, near the hypothalamus and on the optic tract. After that surgery, I was in sympathetic mode for about a year and a half. It was intense. I was always alarmed and anxious with school performance anxiety. I was exhausted, but at the same time, I had the energy to do more than I could afford. Furthermore, I gained 20kg in 6 months despite eating well. This was traumatic for me. Even though I did everything I could to not gain weight, the weight still went up. I felt powerless and I was pissed off. I did a thousand diets and I still fight to lose weight. I have been on a diet ever since.
In 2010, I got an Epstein-Barr viral (EBV) infection. Next, I developed Hashimoto thyroiditis and lost a lot of hair. My beautiful hair that was soft and silky, became sparse, few and very thin. I also had pain in my neck for two years. After that EBV infection, I started to feel tired all the time, but still managed to go out and go to school
In 2011, after a month and a half of pain in the lower back and abdomen, I had a fecal analysis done and found that I had parasitic infection called blastocystis hominis. The doctor gave me metronidazole (Flagyl) in a very high dosage. When the pain in my right leg appeared, the suspicion that it was appendicitis became certain and they operated on me. The surgeon told me my appendix was was 12 centimeters, inflamed and had two abscesses.
In 2012, I had some months of extreme fatigue and abdominal pain. The seizures I had before my brain surgery returned, as did my inability to study due to lack of concentration. I then discovered that I had another parasitic infection, this time giardia. I was treated with Flagyl again. After Flagyl, I was infection-free for 6-7 months.
In March of 2013, I developed an acute onset case of what the doctor’s called a severe case of chronic fatigue, fibromyalgia, and dysautonomia. I had brain fog and was unable to focus. I had tingling in my neck arms. I started gaining again. I have episodes of dysautonomia with vagal crises that include palpitations and tachycardia so strong that even moving around in bed accelerates my heartbeat. Add to all of this a plethora of other minor symptoms. In particular, I have become unbearably cold. Previously, I was the the person who was always in half sleeves. I have also mood swings that sometimes make me feel crazy (such as unexplained nervousness attacks). I felt I had no energy in my muscles and that I could not do anything. Even though and above all I was a girl full of energy and always very cheerful.
Failed Attempts at Healing
Since then, I have done many different types of therapies (homeopathy, mineral and vitamin integrations, neural therapy, micotherapy, osteopathy) with small and short improvements. In 2017, I did probably one of the stupidest things I’ve ever done before, I fasted for 16 days. I was convinced of the idea that it could cure my thyroiditis. After that, I started not digesting well, so much so that if I ate a little more than I should, I was throwing up, and the cold in my body became even more unbearable.
A few years later in 2019, after years of GI problems, that included gastroparesis/delayed stomach emptying, bloating and pain, I was diagnosed with SIBO (sulfur). I was given Rifaximin. I also tried a herbal therapy for SIBO, and for candida, which I also had, and NAC. Nothing worked.
Where I Am Now
I still have most of these conditions. Some symptoms have passed but new ones have emerged. Overall, I am better than in 2013 when CFS started and I just couldn’t get out of bed.
A few months ago, I discovered Dr. Lonsdale’s work on thiamine deficiency and I bought his and Dr. Marrs’ book: Thiamine Deficiency Disease, Dysautonomia, and High Calorie Malnutrition. I believe many of health issues involve thiamine deficiency.
I began with 15mg thiamine HCL injections daily for about two weeks and then increased it to 30mg per day. I also take B complex, magnesium, seleniomethionine, molybdenum, vitamin C, vitamin D, omega 3, zinc and copper because they were low in my blood exam. The first month I also took SAMe with many benefits, but now it seems to make things worse.
I eat only organic food. I don’t eat sugar, processed food, junk food, gluten, milk or dairy products, or alcohol. I have only one or two espressos per day and I eat a lot of apples because they are low in oxalates.
Thiamine Reaction or Something Else?
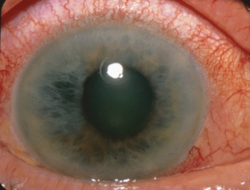
When I woke up on day 2 of thiamine, I saw that my eyes were swollen like balloons, there were some itchy blisters on my eyelids and around the eyes. In the morning other blisters appeared on my elbow and behind my neck under my hair. The morning of day 4, I woke up with a skin rash near the hip.
At the beginning, I had thought these reactions were relative to the thiamine, but I later realized that the hives and swelling were linked to the inositol hexanicotinate, a niacin substitute in the B complex. I have no problems with niacin though, just the inositol hexanicotinate form. From that episode forward, I began taking all the B vitamins separately.
After 2 months of thiamine HCL, I added allithiamine. I began with 1 pill, 50mgs, and I added another 50 mg pill every week, until I reached 300mg. Initially, all the symptoms I had at the beginning of the disease reappeared: severe myalgic attacks in the leg or abdomen, abdominal pain, other pains and unbearable cold in the whole body, especially in the hands. The chills are so severe that I am often shaking. It is so severe that it paralyzes me. This shaking disappeared in a few weeks, but sensation of being cold still persists. And I am still very tired.
After Six Months of Thiamine Therapy
There are some improvements from since I started with allithiamine. For example, my fatigue has improved. Although I always have chronic fatigue, there are times when I feel better for a few hours. Before starting the thiamine, I had frequent attacks of voracious hunger during which I never felt full. I’ve always tried to ignore them, because if I’m not on a strict diet, I am gaining weight. Since taking thiamine, this happens much more rarely and my sense of fullness has improved. Finally, I have fewer nervous attacks. My digestive system seems to be little better. What I am currently taking:
- Allithiamine – 300mg
- Riboflavin – 320mg
- Niacin – 100mg
- Pantothenic acid – 200mg
- Pyridoxine – 20mg
- Myo inositol – 2gr
- Biotin – 5000mcg,
- B12 – until a few months ago. It was low and now it is high.
- Zinc – 30mg
- Copper – 2mg
- Omega 3
- Inulin – 2gr
- Keppra – 250mg x2 a day
- Molybdenum – 200mcg
- Seleniomethionine – 200mcg
- NAC – 1200mg
- Magnesium malate – 1800mg
- Magnesium citrate – 1500mg
- Vit C – 2gr x5 a day
- Lysin 1gr
- Vit D – 10000 UI
- M2MK7 – 100mcg
- DHEA – 50mg
- Maca powder – 5gr
- CoQ10 – 100mg
- LDN therapy – since March 2020
I still have the symptoms of the paradox effect. It has been almost 6 months since I started thiamine, how is it possible? The worst symptoms now are fatigue, frozen hands, shivering. Is the thiamine not working or is something else going on? Could it be that the thiamine revealed some other deficiency that is causing me this reaction? I’d like to know whether I should continue to take it.
A warm hug from Italy.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on May 17, 2021.