I live in a retirement home and I see many residents who are receiving nasal oxygen, so I am going to try here to address the reason. They may have been diagnosed with either heart disease or lung disease and they have probably been observed clinically to be “short of breath”. Of course, I do not know the specific reason for a given individual receiving this treatment, but does the average patient understand why he or she has to tolerate this inconvenience? I strongly suspect that they have merely been told that they need oxygen administration without explaining the underlying reason. Generally speaking, most people take for granted that they are alive and have little interest in why or how, unless their health becomes threatened. Obviously, when nasty things start to occur, they ask a physician why it is happening to them and the physician tries to diagnose the affliction. It usually winds up by the patient being told that it is disease A or B and a superficial description of the disease is provided. Each disease is regarded as having a specific treatment and a specific cure that is usually being sought by a drug company. The most up-to-date drug is offered. Unfortunately, with the exception of bacterial infection, most drugs only treat the symptoms and do not address the underlying cause. Modern research focuses almost exclusively on genetics and for the most part little consideration is given to prevention other than making a diagnosis of early disease. So why are these people receiving nasal oxygen?
Why Do We Need Oxygen?
Of course, we all understand that our environment must supply us with oxygen, water and food, without any of which we die. Although I have written about oxygen utilization in many posts on this website, it bears repetition because of what I want to say about nasal oxygen administration as described above. First of all, it must be stated that the main three gases in air are nitrogen, oxygen and inert gases. Seventy-eight percent of air is made up of nitrogen, 21% is oxygen, just under 1% is argon and the remaining part is made up of other gases such as carbon dioxide and water vapor. In other words, our oxygen intake is dosed. Too much oxygen is as lethal as none at all, illustrating the wisdom that was propounded in ancient China called Yin and Yang, not too much and not too little. The thing that always amazes me is the concise nature of the natural world and how we should fit into it. The more I get to know about the human body the more I realize how little we know. However, we do know what we do with oxygen. It is called oxidation.
Understanding Oxidation
It is surprising to me that many people appear not to understand that when a fuel burns, it is because the fuel is combining with oxygen. The result is the production of energy in the form of heat, the simple physics that we learned in school. The word oxidation is defined as “cause to combine with oxygen”. But consider that a piece of newspaper will not burst into flame by itself. It has to be ignited. If we use a match, the heat generated from striking it on a rough surface is enough to make it burst into flame and that energy in the form of the flame is transferred to the newspaper. What we are looking at is simply the transfer of energy from one action to another. Even striking the match requires the energy of the individual who performs it. But there is another factor that comes into play here. The newspaper will produce what we call ash, representing the fact that the newspaper has not been completely consumed (oxidized). I am providing these simple principles to explain now that this is exactly what happens in the body. The principles are identical: the mechanisms are different.
Cellular Oxidation
Starting with first principles, as we breathe, our lungs are taking in air and extracting oxygen from it. The oxygen is transferred into the bloodstream and picked up by combining with hemoglobin that coats red cells. This represents a transport system and the oxygen has to be delivered to each of the 70 to 100 trillion cells. This in itself is an amazing representation of the blood circulation. The deoxygenated blood is transferred to the venous circulation and transported back to be re-oxygenated. It is now that the process of oxidation takes place in the cells that have received the oxygen. To put it as simply as possible, glucose, the primary fuel, combines with oxygen to yield energy that drives the function of the cell in which the oxidation takes place. Just like the analogy of the newspaper, the combination of glucose with oxygen has to be “ignited”. Thiamine and other vitamins and minerals are the equivalent of a match. Carbon dioxide and water are the equivalent of ash from the newspaper. They have to be got rid of and so they are expired in the breath. Gasoline in a car engine has to be ignited so the explosion in a cylinder might be referred to as oxidation. The smoke in the exhaust pipe is the “ash”.
Nasal Oxygen and Hypoxia
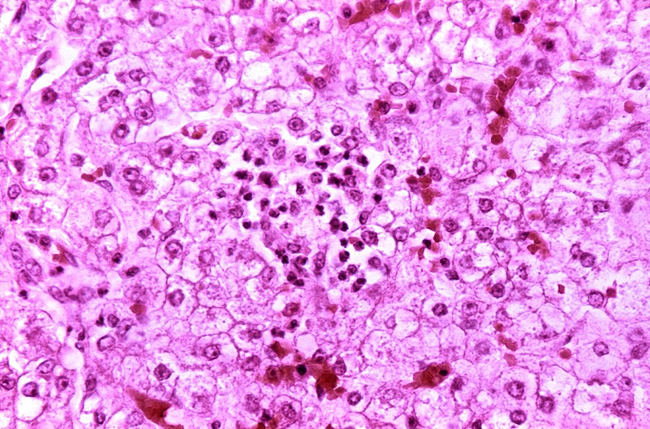
It is my experience is that the use of nasal oxygen, although completely correct in itself, seems to be associated with ignorance of the fact that the sufferer is probably lacking the vitamins and minerals that enable the oxygen to be utilized in the body. Indeed, the lack of vitamins and minerals may be the main issue in the underlying cause of the disease, a fact that is flatly denied by the vast majority of physicians. The word for lack of oxygen in medical literature is hypoxia. The effects of thiamine deficiency, because it causes exactly the same symptoms, is referred to as pseudo-hypoxia (false lack of oxygen). In reality, the symptoms of the patient are caused by lack of oxidation, resulting in lack of cellular energy and consequently, their loss of function. Using the above analogy, it would be like holding a piece of newspaper and expecting it to burst into flame spontaneously. The most recent medical literature is full of manuscripts reporting the relationship of thiamine deficiency with chronic disease, even cancer, and various forms of traumatic surgery. It is not sufficiently recognized that the widespread ingestion of empty carbohydrate calories easily induces inefficient oxidation. This is but another reason why Dr. Marrs and I have written our book “Thiamine Deficiency Disease, Dysautonomia and High Calorie Malnutrition“, available at Amazon books. ‘
Conclusion
Why do so many individuals require nasal oxygen? With the present thought process, the patient is considered to have a condition that would benefit from its administration, perhaps heart or lung disease, operating on the present disease model. Physicians are not really thinking in terms of oxidative metabolism as the underlying mechanism. The point that we are trying to make here is that no amount of extraneously supplied oxygen will be effective unless the vitamins and minerals are present in sufficient quantity for the oxygen to be used in the creation of energy. Oxidation requires the presence of glucose, oxygen and the requisite vitamins and minerals and deficiency of any one of the three will be responsible for the symptoms.
We Need Your Help
Hormones Matter needs funding now. Our research funding was cut recently and because of our commitment to independent health research and journalism unbiased by commercial interests we allow minimal advertising on the site. That means all funding must come from you, our readers. Don’t let Hormones Matter die.
Yes, I’d like to support Hormones Matter.
This article was published originally on April 5, 2018.