I recently stumbled upon on a research paper published in 1968. It was not that long ago in the overall course of modern medicine, perhaps even its heyday, when all things were still possible and before the complete fealty to pharmaceuticals arrived. To the youngsters and to those coming of age in the last 20 years, however, anything published pre 1990 is ancient history. What could such old paper tell me about medicine that is new and useful? It turns out an awful lot.
Back in the day, research was a little simpler and more focused, not on finding out which drug could be fit to which symptoms, but on how things worked. Good experimental design, answered mechanical questions, like if we apply X to Y or if we remove X from Y what happens?
In this paper, Encephalopathy of Thiamine Deficiency: Studies of Intracerebral Mechanisms, the researchers identified a very important component about Vitamin B1/thiamine deficiency – the time course of the disease process. That is, with a diet deficient in thiamine, how long does it take before symptoms emerge, what is the corresponding level of deficiency in the brain, and at what point, after supplementation, does recovery begin; important questions clinically.
Vitamin B1 – Thiamine Deficiency
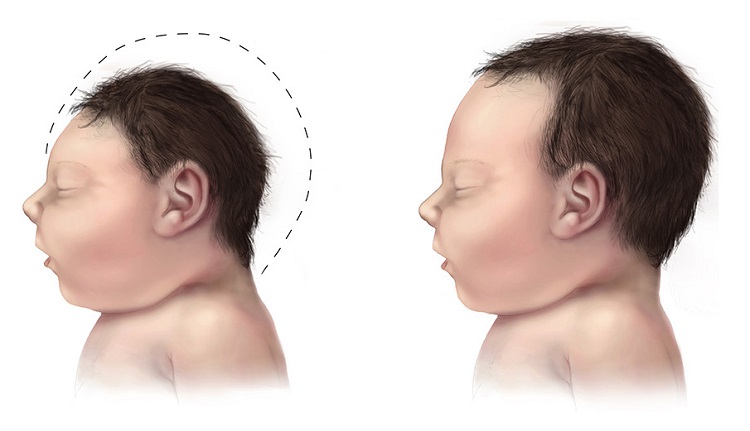
Remember, vitamin B1 or thiamine deficiency at its worst is linked to severe decrements neurological functioning, like Wernicke’s Encephalopathy that include noticeable ataxic and gait disturbances (loss of voluntary control of muscle movements, balance and walking difficulties), aphasias (language comprehension and/or production difficulties), and if it persists, Korsakoff’s Syndrome (severe memory deficits, confabulations and psychosis). Thiamine deficiency was originally observed in only chronic and severe alcoholics or with severe nutritional deficits as seen in famine. Fortification of food stuffs was thought to relieve much of the nutritional risks for deficit, especially in impoverished regions. More recent research, however, indicates that thiamine deficiency has reared its ugly head once again and this time in modern, non-impoverished, regions where the food supply is ample. How can that be?
Non-Alcoholic Wernicke’s Encephalopathies
Thiamine deficits can be mediated by a number of factors, including by less obvious nutritional deficits where food supply is abundant but nutrition is lacking (a diet of highly processed, carbohydrate and fat laden foods), with thiamine blocking factors found in medications/vaccines, environmental toxicants and some foods, after bariatric surgery and in disease processes like AIDS. Over the course of our research, thiamine deficiency has been observed in previously healthy, young, non-alcoholic patients, post medication or vaccine, along with symptoms of dysautonomia.
What has always struck me about the thiamine deficits we observe is the differential expression and time course of the symptoms. In some people, the reaction leading to thiamine deficit appears linear, progressive and rapid. In others, the symptoms appear to wax and wane and to evolve more slowly. How is that possible? Certainly, individual predispositions come into play. Some individuals may be somewhat thiamine deficient prior to the trigger that initiates the full expression of symptoms, while others have higher baseline stores. Additionally, anti-thiamine environmental exposures and other medical conditions/medications may also come into play. In the literature, however, the progression of symptoms from bad to worse is almost always direct and rapid, perhaps mistakenly so. Indeed, Wernicke’s Encephalopathy is a medical emergency necessitating immediate IV thiamine. How is it then, that we see more chronic, remit and relapse patterns of thiamine deficiency, even in some cases where thiamine concentrations are being managed medically?
Cerebral Thiamine Deficiency: Crossing the Black Line
It turns out, there is black line with regard to thiamine deficiency, that when crossed overt symptoms emerge, and a similar black line, that demarks recovery. It is possible then that barring a continuous blockade of thiamine, one can move above and below those lines and the corresponding symptoms may wax and wane. The paper from 1968, cited above, found those black lines, in rodents, but we can extrapolate to humans.
The research. The investigators took three groups of female rodents, a paired group of thiamine deprived and thiamine supplemented, along with a group fed ad lib (as desired) and assessed the time course and concentrations of cerebral thiamine deficiency relative to the initiation and progression of the observable neurological symptoms associated with Wernicke’s encephalopathy in rodents (ataxia, loss of righting, opisthotonos –rigid body arching). The experiment lasted about 6 weeks.
Neither the control group (thiamine supplemented) nor the ad lib group demonstrated neurological deficits at any time during the study. The thiamine deprived group, on the other hand, demonstrated symptoms that began with weight loss, progressive anorexia, hair loss (recall our observations about hair loss) and drowsiness at about 2.5 weeks into the experiment. Interestingly, no neurological signs of thiamine deficiency were seen at that time.
The results. At 4.5 weeks in, the researchers noted a rapid progression of symptoms and decline of health over the course of the next 5 days (the black line). These symptoms included: incoordination with walking, impairment of the righting reflex, reluctance to walk, walking backwards in circles, imbalance, rigid posturing and eventually a total loss of righting activity and severe drowsiness.
One can imagine, if a similar deprivation of thiamine were observed in humans, the corresponding symptoms might also include the initial hair loose and weight loss, perhaps noticeable, perhaps not depending upon the time frame and severity of the thiamine deficiency. It would also include incoordination and difficulty with walking, balance and voluntary movement, perhaps tremors, excessive fatigue or sleepiness and the myriad of neuro-cognitive disturbances noted in Wernicke’s syndrome.
In the cited experiment, one injection of thiamine reversed these symptoms to a nearly normal, or apparently normal neurological state within 24 hours.
Brain Thiamine Thresholds
Animals from each of the groups were sacrificed and examined at each of the stages of the experiment. Brain thiamine and other markers of thiamine metabolism were assayed to determine the cutoff levels of thiamine that demark symptoms and recovery. This is really interesting and the beauty of this entire study. Neurological symptoms become apparent when cerebral thiamine concentrations reach 20% of normal. Recovery begins when those concentrations climb to 26% of normal. At least in rodents, one has to deplete 80% of the brain thiamine stores before overt neurological symptoms become apparent; 80% – that is a huge deficit. Similarly, it doesn’t appear to take much to right that deficit, only a 6% increase in thiamine concentration set the course for improvement.
If we extrapolate to humans, where life span, genetic and environmental factors likely moderate the degree of thiamine stores and consumption, we still contemplate a rather large thiamine deficit needed before overt symptoms of Wernicke’s emerge. Similarly though, it is also evident that a rather small change in thiamine can have enormous effects on neurological functioning. In the case of the rodents, a mere 6% point change reversed the symptoms. One might suspect equivalent deficit/recovery thiamine parameters in humans.
Waxing and Waning Symptoms: A Case for Persistent Thiamine Deficiency
If we consider the possible course of non-alcoholic thiamine deficiency, where no extraneous variables like bariatric surgery or thiamine deficient parenteral feeding are present and where dietary thiamine varies daily and is not held constant as it is during experimental conditions or during famine, we can begin to see how thiamine related neurological symptoms may wax and wane. Different exposures and triggers may decrease thiamine periodically, even to the point where overt neurological symptoms present. When those exposures are removed and barring deficiencies in metabolism and diet, symptoms may abate, at least temporarily, and until the next trigger or until the black line is crossed anew and thiamine deficiency becomes the medical emergency observed in overt Wernicke’s.
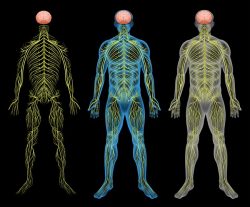
In contrast, the more persistent or chronic thiamine deficits that do not cross the 80% depletion cutoff (or the human equivalent), may also wax and wane and show all the core neurological symptoms expected in overt Wernicke’s though to a much lesser degree. Additionally, as we have speculated, persistent thiamine deficiency might disable mitochondrial functioning in such a way that the patient presents with a myriad of seemingly unrelated symptoms, that are not typically attributed to thiamine deficiency, such as cardiac dysregulation, gastroparesis, autonomic instability, demyelinating syndromes and hormone irregularities, especially thyroid, but also reproductive hormones. These too may be related to thiamine deficiencies. Although, we cannot and should not rule out other causes as well, sub-optimal thiamine may be involved with a host of complex disease states and medication adverse reactions where neurological symptoms are present. Thiamine deficiency should be tested for and ruled out before more invasive therapeutic options are contemplated.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.









Hi.
Is there any evidence that Thiamine stops hair loss?
Hello ..lm reaching out in desperation. Maybe hoping for some direction. Low income women now 50 hysterectomy had anxiety at young age poor diet , pcos, believed to be insulin resistance…hit with ebv and viruses, hairloss for 10 year tho Dr say tsh if fine l experience internal vibrations after covid or Vax unsure believe l experience dysautonomia or autonomic nervous system stuff .. cold and hot eyes blurry, fatigue, eye floaters, moods, hard time to focus and read . How can one start getting better please. Never took vitamins told it bad and synthetic. I do take magnesium biglycinate and nac now .how can someone who’s low incone get better any step by step or vitamins to slowly start but won’t make me worse . I’m single no help at all
The easiest and least expensive way to help would be clean up the diet as much as possible. Cooking from scratch is often far healthier and cheaper than buying/eating pre-cooked processed foods. A good paleo-like cookbook, a crockpot, and lots of storage containers (glass, if you can) and you can cook a week or two worth of food, freeze it and have meals ready to go. Thiamine hcl, which is the type found in most over the counter or amazon vitamins is also relatively inexpensive. Bluebonnet vitamin B1 is a good brand and they are 11 dollars a bottle for 100 at 100mg. A solid multi-vitamin would be helpful too, although the good ones are much more expensive I am afraid. Maybe start with the thiamine and cleaning up the diet and go from there.
Dear Dr. Marrs!
I’ve been eating a paleo diet the last 2 years and also experienced a lot of stress and was mentally as well as physically very active. I was probably undereating and found out the there weren’t hardly any sources of b1 in my diet. I’ve been experiencing a lot of symptoms which could be related to thiamine deficiency (although some of these symptoms I already had before this time). I was already checked by a neurologist, they also did an MRI, checked B1 in whole blood and didn’t find anything.
They said to me that I don’t have to worry about it being Wernicke’s Encephalopathy, so I really hope that’s true (therefore I didn’t get Thiamin i.v.)!
Nevertheless I am really concerned and not really sure what I should do about it, do you have any suggestions? I don’t think that I can get thiamine i.v. in my place and because I live in Europe I also can’t find allithiamine.
Do you think it would be okay to take high dose benfotiamine or Thiamin HCL to reverse my symptoms? Because I think with high dose oral Thiamine HCL one could also achieve pretty high plasma levels (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3293077/), (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3293077/figure/F2/)?
Would this be sufficient to penetrate the blood brain barrier enough if at all?
My symptoms are pain in the calves, slight gait unsteadiness and problems with balance with closed eyes, brain fog, slow thinking, slight drowsiness, poor emotion control, poor concentration, fatigue etc…
Do you think if it’s due to b1 deficiency that my symptoms are reversible?
Would really appreciate a response and thank you a lot in advance!
with best regards
Sem
Is there a test, or method of diagnostic, if the subject is 8 year old? I am researching relation to the Basil Ganglia. Symptom parallels are shutdown/anxiety/shyness, studdering (which several people mention thiamin having a positive effect with studdering.)
Christopher, unfortunately, the lab we used is no longer available and the tests at conventional labs are generally insufficient. The expert on all things thiamine, especially pediatric, is Dr. Derrick Lonsdale. We have several of his articles on our site, including one about lab testing, just put his name in search bar. On the web there are articles as well.
Thank you for the information, I look forward to doing some reading! I interestingly, I found your article while researching the topic, and see that you happen to me here in Las Vegas too, so it’s a nice coincidence. Do you know if there happens to be a SPECT imaging machine in Las Vegas (or one on the way)?
Alternatively…. what are your thoughts on that technology as a diagnostic tool?
You’re welcome. I don’t know if thiamine will help w/ stuttering but since so many folks, children especially, are thiamine deficient (a lot of the vaccines leach thiamine), it will likely help with overall health. If you use it and it does help, please let me know. We’ll write about it to let others know.
Regarding the spect imaging, I have not been in that area for a while, although if anyone is using those, I would guess it would be Cleveland Clinic. They have a lot of cool toys and do some interesting research. Unfortunately, their focus is on the elderly. I don’t know that they do work in pediatrics, at least not here in Vegas.
Dear Dr. Marrs, Are you aware of any lob currently doing the thiamine testing recommended by Dr. Lonsdale?
Margie, unfortunately not. The lab previously used is no longer and we haven’t been successful finding another. It seems only to be used in research.