I became a “sitting duck” for the hysterectomy industry after experiencing a day of unremitting abdominal pain. Having never experienced female problems before, this had me concerned. So off I went to my gynecologist, a man I’d respected for 20 years, the man who’d treated me for infertility and saved me from another c-section by doing VBAC (Vaginal Birth After C-section). So the stage was set.
An ultrasound showed a large, complex ovarian cyst. My gynecologist said that “everything must be removed” and scheduled surgery. Of course, I was in shock and didn’t even know what to ask. He referred me to an oncologist for consultation who said he couldn’t tell if it was cancer and then quickly disappeared giving me no chance to ask questions. I went back to my gynecologist with a list of questions asking why I needed other organs removed. Unbeknownst to me, I was lied to about my condition (as later discovered from my medical records).
Although my barely audible inner voice told me something wasn’t right, I dismissed it telling myself that I had a good, reputable doctor who wouldn’t needlessly remove organs. I also convinced myself that a surgery that’s so common can’t possibly be all that bad. And ovarian cancer is often deadly. I mistakenly listened to family and friends who urged me not to delay surgery.
Fast forward to the day of surgery: There were residents surrounding my bed in pre-op. I didn’t recall this ever being mentioned or on any of the “consent” forms. I didn’t even know it was (is) a teaching hospital because it’s not affiliated with any university.
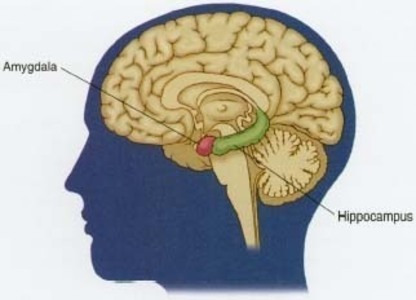
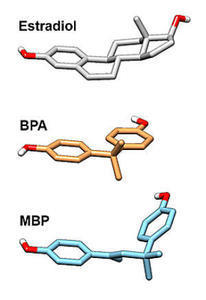
The surgical recovery was easy for me. However, it became clear very quickly that I had become a different person. I felt like my HEART and SOUL were removed in that operating room. Despite being prescribed estrogen, everything fell apart. I quickly spiraled into a suicidal depression, couldn’t sleep more than two or three hours at a time, with a lengthy list of symptoms of hormonal deficiency and endocrine havoc. I also developed rather severe diarrhea. By 4 months post-op, I’d aged about 15 years from massive hair, skin collagen, and muscle mass loss. Yet a call to my gynecologist/surgeon resulted in being told “we’ve never heard of those problems before” followed by the phone being hung up. He’d now abandoned me as his patient.
I could barely function and was holding onto my job by the skin of my teeth. I became a recluse going to great lengths to avoid running into people. And when I did, I could see the shock on their faces. Thankfully, my husband took on the household and minimal child care duties (my children were older) but I missed out on years of my children’s lives. Once I finally found a doctor who would “dole out” more estrogen, I could at least do basic daily functions. But the taken-for-granted, joy-filled days from when I was intact seem to be gone forever. I don’t even have the strong feelings of love for my family any more. Seven years after that fateful day, I still mourn the many losses caused by the removal of the organs that were so essential to every aspect of my being, the ones that made me female in every sense of the word.
What I found in my medical records and through research was eye-opening. All my female organs were removed to help gynecology residents meet their surgical requirements. Sadly, Graduate Medical Education (GME) accreditation requirements emphasize hysterectomy to the exclusion of organ-sparing procedures. And the hospital’s GME website stated that hysterectomies are the “bread and butter” of gynecological training.
I wonder how much my gynecologist was paid to train these residents? My records from the oncologist show that he enabled my gynecologist. I also question what was submitted to my insurance company for them to authorize “hysterectomy” because there was absolutely NOTHING wrong with my uterus (or my other ovary). Based on all my research and the experiences of scores of other women, if one female organ is being removed, it’s acceptable to remove them all. Insurance authorization and hospital consent forms are designed to allow this. This doesn’t make sense. I wonder if prostatectomy consent forms allow removal of testicles?
The hormonal effects of ovary removal are far more understood and acknowledged. But the anatomical and skeletal effects, not so much. So my next article will talk about these changes.
Hormones MatterTM is conducting research about hysterectomy. If you have had hysterectomy, please take a few minutes to complete this important survey. Then share the survey link with all of your friends. These data could save the life of another women. The Hysterectomy Survey.
To learn more about our research, click Take a Health Survey and sign up for our newsletter for updates on the latest research and new surveys.