History of Gut Pain and Epigenetic Malnutrition
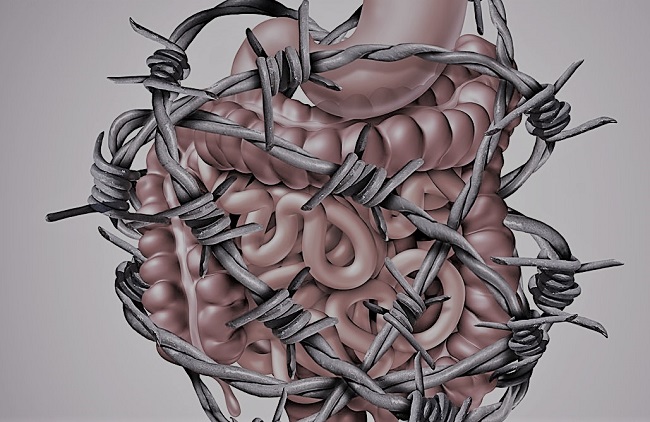
I am 32 years old and have suffered from ill health all of my life. From as long as I can remember, I’ve experienced gut pain, fatigue, and hyper-sensitivity. If there was something to catch, I would catch it. I react to everything and suffer chronic gut and nerve pain.
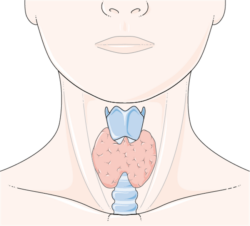
As a young child, I had chronic abdominal pain in the lower right quadrant and would often be buckled over in pain. Doctors thought it was appendicitis so removed my appendix but the pain continued. I was chronically tired and sensitive to the cold. I would struggle to get up in the morning to go to school and would stand in the shower dousing myself in hot water for as long as I could to warm up my body. Cold hands and feet has continued into adulthood.
I was born into a family that struggled with spine, neck, head, and gut issues. I was raised on cow’s milk and barley formula as my mother was unable to breastfeed. My mother and aunt had Ehlers Danlos Syndrome. I was diagnosed with it 8 years ago. My mother has Arnold Chiari malformation, my aunt scoliosis. They were post-war children. My grandmother had spinal issues and likely was very deficient in the B Vitamins. My grandfather, aunt and mother all suffered from gut issues, my grandfather eventually dying from bowel cancer. He was sensitive to many foods, particularly FODMAP rich ones.
I had many allergies – dust mite, grass, cow’s milk etc. I suffered an adverse reaction to the MMR vaccine when I was eight – with an intense full body rash. I was bedridden with intense fatigue for two weeks. Around the same time, tests found huge numbers of the parasite dientamoeba fragilis (D fragilis) in my stool. Dientamoeba fragilis together with Blasto hominis, another intestinal parasite, have been found in large numbers in my stool ever since. Despite trying many things, I’ve never been able to get rid of them.
Increasing Food Sensitivities, Weight Loss, Amenorrhea, and Osteoporosis
By the age of ten, I was struggling with depression and increasing sensitivities to many foods – particularly gluten and dairy. The only thing that seemed to help was exercise. I played competitive soccer, did cross-country and athletics and rode my bicycle everywhere. At this time, I started becoming vegetarian, in response to my growing concern about the state of the world, animal cruelty and the environment. This meant consuming a lot of gluten and dairy based foods. As I entered puberty, my body couldn’t keep up with the energy demands of this stage of development and I began losing weight rapidly, despite eating a ton of carbs.
I was working hard at school, and have always pushed myself to succeed, but as my body became more and more unwell, I struggled with focus and concentration. My depression became worse and the world felt very bleak. Everything I ate caused pain, bloating, and fatigue. I was eating lots of pasta and cheese to try to fuel my sports but I continued to lose more and more weight. Throughout my parents had been doing everything to investigate and treat the cause of the illness, but I just kept getting more and more unwell. My weight dropped dangerously low, I developed bradycardia and I struggled to think clearly.
The years passed through adolescence and into early adulthood. Through sheer willpower and making myself eat, despite the intense pain it caused, including severe abdominal cramping, sulfur gas, burning, over-heating, swelling, headaches and more, I could get some extra weight on for a while, but it would quickly fall off again. My growth and development suffered. My bones froze in time – a bone age at 19 showed the bones thought they were 13. I had amenorrhea. I developed osteoporosis. An endoscopy showed an inflamed caecum and inflammatory spots in my sigmoid colon.
Through my teenage years and twenties, I had to follow extremely restrictive diets. I had to quit being vegetarian, as it didn’t leave anything to eat and my body clearly needed nutrients from animal foods to survive. I reacted to FODMAPs, histamines, too much fat, too many carbs – there was so little I could eat without feeling extremely unwell.
I would often experience intense nausea attacks, severe bouts of sudden pelvic pain, stomach bugs, and caught giardia several times. I got shingles at the age of 21, a strange fever induced by tick bites at 22, and viral meningitis at the age of 26.
Gut Dysmotility, Progressive Neuropathy, and Migraine
My gut was becoming lazier and lazier. At the age of 23, I wound up in emergency in extreme abdominal pain after it stopped moving altogether and my intestines became fully impacted. The pain was excruciating. Eight sachets of heavy duty laxatives did nothing to the situation. I was started on prucalopride (an enterokinetic drug) to help get it moving again. I cannot function without this drug now. When I stop taking it, my gut ceases to move altogether.
Through my twenties, I also started suffering from tingling in my arms and legs and increasing peripheral neuropathy. By the age of 27, I would experience episodes where an entire arm or leg was completely numb. Blood work showed my B12 had dropped very low. I went on B12 injections and increased food sources of B12. Things improved for a while but then the neuropathy returned. I subsequently developed Reynaud’s syndrome.
Around the same time, I started developing worsening headaches and a few years later migraines. The migraines were so bad I couldn’t move without intense vertigo and extreme nausea. I had to lie in a pitch dark room and wait it out. Some migraines were preceded by a confusional aura where I couldn’t tell what anyone was saying to me. I could understand the individual words but not when they were strung together in sentences. The vertigo continued for about 6 months.
Exercise became more painful too. Despite being fit, I would suffer from intense DOMS, headaches and nausea after running. Muscles started becoming more and more sore and painful despite taking electrolytes, being careful about my nutrition and warming up and down.
I woke up every morning feeling exhausted and sleep studies revealed I had developed sleep apnea – something I had thought wasn’t so common in women of my age and build.
Stress Fractures, Worsening Neuropathy, and Hypoxia
Earlier this year, I wound up with a bad stress injury in my hip – several stress fractures in my femoral neck despite no blow to the area and no fall – which doctors thought quite unusual for someone of my age who was running low mileage recreationally. The injury brought with it chronic nerve pain along my right side on top of worsening neuropathy.
I would wake up in the middle of the night with numb limbs. Nerves would fire spontaneously in my legs and arms. Nerves in my jaw felt constantly stimulated and my tongue would swirl uncontrollably around in my mouth. My gut stopped moving more and more frequently and I would have to take laxatives regularly to clear it out.
I had severe GI burning and was unable to eat anything other than clear broth and coconut water without pain. An endoscopy found bleeding in my sigmoid colon. My hemoglobin dropped 17 points and I struggled with breathlessness, unable to get up a flight of stairs or even walk a few hundred meters without feeling deeply exhausted.
To date, I have been diagnosed with POTS, Ehlers Danlos Syndrome, dysautonomia, gastroparesis, severe osteoporosis of the lumbar spine, and peripheral neuropathy. This comes against the backdrop of the gut problems experienced since childhood. These other health issues were, to no small degree if not caused, then significantly worsened by my gut issues. I have had long periods of time where I couldn’t absorb food or eat very much due to my gut problems, so I have been underweight for most of my life. As a result, I am likely deficient in many nutrients.
Current Diet, Activity, and Recent Testing
Diet
- Breakfast: steamed greens (e.g. some combo of broccoli, beans, spinach, asparagus, etc.), 1-1.5 scrambled organic egg, 1 cup bone broth with 1 desert spoon collagen peptides + 1 desert spoon seaweed.
- Lunch: 1 cup bone broth with 1 desert spoon collagen peptides + 1 desert spoon seaweed with 1 egg yolk stirred through OR some homemade chicken liver pate on carrot sticks instead of the egg yolk; 1 raw carrot and/or raw cucumber sticks; sometimes 1 packet of roasted nori.
- Snacks: 1 glass homemade carrot, celery and ginger juice; some blueberries and/or a kiwi fruit.
- Dinner: some protein (e.g. half a single piece of salmon, 8 prawns, small amount of red meat), green veggies (e.g. steamed beans, asparagus, spinach, broccoli), a starchy veggie (e.g. pumpkin, sweet potato, beetroot), sometimes some green salad.
- After dinner: a few blueberries and/or pieces of mandarin, 30-40g vegan carob (cocoa butter, carob powder, no sugar), a cup of herbal tea.
Activity and Exercise
- Daily: walking – approx. 12-13km over the course of a day including daily activities, as measured on Fitbit.
- Running: 3x per week – currently at 9km total over the week; very slow 6’20” pace.
- Yoga: 2x per week 1hr classes – beginner.
- Physio: 3x 20-25min per week – core exercises for lower back, hips, shoulders etc as set by exercise physiologist.
Recent Testing
These tests were conducted by RN Labs and Great Plains Laboratory before I began thiamine.
Stool – GI-360
- Klebsiella pneumoniae – very high
- Proteobacteria – very high
- Akkermansia muciniphila – very high
- Escherichia spp. – very high
- Bacteroides spp. – very high
- Endolimax nana – very high
- Eubacterium siraeum – very high
- Enterobacter cloacae – high
- Elastase – low
- Butyrate – low
- Clostridia – very low
- Faecalibacterium prausnitzii – very low
- Veillonella spp. – very low
- Secretory IgA – very low
Urine – Organic Acid Test
Yeast and fungal markers:
- 3-Oxoglutaric – 0.69 (<0.33) – Elevated levels of 2-Oxoglutaric suggest dietary vitamin deficiencies or supplementation with 2-ketoglutaric acid. Coenzyme A (derived from pantothenic acid), flavin adenine dinucleotide (FAD) (derived from riboflavin), and thiamine are required for conversion of 2-oxoglutaric acid to succinyl-CoA.
- Arabinose – 70 (<29) – Urinary levels higher than the reference range may simply reflect a high dietary intake of these fruits. However, arabinitol (which converts to arabinose) is also documented to be produced by the Candida genus of yeast. When elevated in body tissues, it can link with lysine and arginine. In theory, this may block some binding sites for coenzyme pyridoxal phosphate, biotin or lipoic acid at the lysyl residue in apoenzyme proteins. This would impair enzymatic processes, such as transamination of amino acids (in spite of “normal” intake of vitamin B6). A finding of high arabinose, without dietary intake of the above-mentioned fruits, suggests a stool analysis or other tests/examinations for Candida overgrowth.
- Tricarballylic – 2.3 (<0.44) – Tricarballylic acid is a chemical by-product released from fumonisins during passage through the GI tract. Fumonisins are fungal toxins produced primarily by F. verticillioides. Tricarballylic acid is an inhibitor of the enzyme aconitase and therefore interferes with the Krebs cycle.
Bacterial markers:
- 4-Hydroxybenzoic – 1.9 (<1.3) – A marker for intestinal dysbiosis.
Oxalate metabolites:
- Glyceric – 16 (0.77-7) – High glyceric levels on an organic acids test usually relates to primary hyperoxaluria type 2.
- Oxalic – 389 (range = 6.8-101) – High oxalic with or without elevated glyceric or glycolic acids may be associated with the genetic hyperoxalurias, autism, women with vulvar pain, fibromyalgia, and may also be due to high vitamin C intake.
Glycolytic Cycle Metabolites:
- Lactic – 51 (<48) – Elevated by a number of nonspecific influences, such as vigorous exercise, bacterial overgrowth of the GI tract, shock, poor perfusion, B-vitamin defciency, mitochondrial dysfunction or damage, and anemia, among others.
Mitochondrial Markers – Krebs Cycle Metabolites:
- Succinic – 24 (<9.3) – The most common cause of elevated succinic acid is exposure to toxic chemicals which impairs mitochondria function.
- Malic – 2.7 (0.06-1.8) – Higher levels of malic acid in urine indicates inefficiencies in energy production. Elevated malic acid values suggest increased need for niacin and CoQ10. When malic acid is simultaneously elevated with citric, fumaric, and alpha-ketoglutaric acids, it strongly suggests cytochrome C oxidase deficiency, indicating dysfunction in the mitochondrial energy pathways.
- Aconitic – 6.6 (6.8-28) – Elevated in mitochondrial disorders. Aconitase metabolizes citric and aconitic acids, and is dependent on glutathione. Increased levels may indicate additional requirement for reduced glutathione.
Neurotransmitter Metabolites:
- HVA / VMA Ratio – 2.3 (0.16-1.8) – An elevated ratio is often the result of decreased conversion of dopamine to norepinephrine by the enzyme, dopamine beta-hydroxylase. This inhibition is commonly caused by Clostridia by-products, including HPHPA, 4-cresol, and 4-hydroxyphenylacetic acid, which are also measured in the OAT.
- Dihydroxyphenylacetic (DOPAC) – 3.9 (0.08-3.5) – DOPAC levels may be elevated due to inhibition of dopamine beta hydroxylase (DBH) from Clostridia metabolites, the mold metabolite fusaric acid, pharmaceuticals such as disulfiram, food additives like aspartame, or to deficiencies of the DBH enzyme due to copper deficiency, vitamin C deficiency, or malic acid deficiency.
- Quinolinic – 0.58 (0.85-3.9)
Ketone and Fatty Acid Oxidation:
- 3-Hydroxybutyric – 5.7 (<3.1) – A moderate urinary increase in 4-hydroxybutyric acid may be due to intake of dietary supplements containing 4-hydroxybutyric acid, also known as gamma-hydroxybutyric acid. Very high levels may indicate the genetic disorder 3-methylglutaconic aciduria involving succinic semialdehyde dehydrogenase deficiency.
- Acetoacetic – 32 (<10) – High levels of acetoacetate in blood may result from decreased availability of carbohydrates (eg, starvation, alcoholism) and/or abnormal use of carbohydrates storage (eg, uncontrolled diabetes, glycogen storage diseases).
- Methylsuccinic – 5.7 (0.1-2.2) – Very elevated values may indicate a genetic disorder. Fatty acid oxidation defects are associated with hypoglycemia, and lethargy. Regardless of cause, intake of dietary supplements containing L- carnitine, or acetyl-L-carnitine may improve clinical symptoms.
- Sebacic – 0.39 (<0.24) – Sebacic acid is a breakdown product of fatty acids. Higher levels can be seen when the breakdown of fats is impaired or blocked. May be associated with Vitamin B2 (aka Riboflavin) deficiency. Riboflavin is needed for fatty acid breakdown.
Nutritional Markers:
- Vitamin B2 – 0.38 (0.04-0.36)
- Vitamin C – 598 (10-200)
Discovering Thiamine
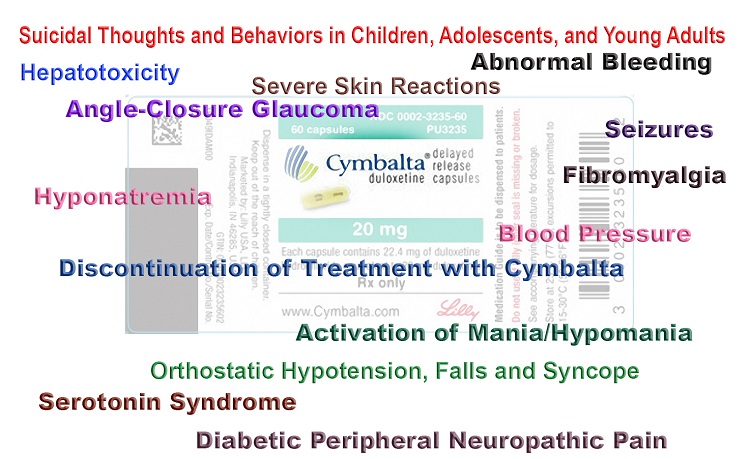
During this time, I was fortunate enough to learn about the work of Dr. Lonsdale and Dr. Marrs and have started talking high dose Lipothiamine. After several months, the chronic nerve pain is reducing and my gut has improved somewhat however I still struggle with pain and am very sensitive to a lot of foods.
I also have been learning more about the role of genetics and epigenetics in my condition. I am compound heterozygous for the MTHFR mutations and also have SNPs of the PEMT, NOS3, COMT, MOAB, GST genes alongside a number of other SNPs (including CYP, PONI, GAD, GGH, HTR2A, MMAB, NAT2, SLC, SULT, ALD, CBS, DHFR, MTR, TCN1, CBS, DDC, DRD and more).
I am currently taking 1000mg of Lipothiamine orally per day. If IV was possible, I would do that given my gut problems, but we have not been able to find anyone able to administer that here in Australia. In addition to the Lipothiamine, I take magnesium (800mg), liposomal Vitamin C (6000mg), glutathione (450mg), probiotics, a multivitamin, cod liver oil, B-complex, Alpha Lipoic Acid, zeolite, zinc and methylated b12 (shots occasionally and drops in between).
I follow the Auto-immune Protocol diet (including all fresh, unprocessed food, no sugar, lots of veggies and fruits, organic fish, meat, eggs, etc.), walk daily, practice yoga, meditation, daily stretching and gentle jogging a few times a week.
Improvement with Thiamine and Outstanding Questions
In recent weeks, I’ve been finding the nerve pain has significantly improved on this high dose (1000mg) of Lipothiamine however my gut symptoms are quite bad – with a lot of GI burning. I experienced this when I first started taking the Lipothiamine but it subsequently subsided so I am unsure if this is something I need to just push through or if I am on too high a dose.
I would love to hear others experience and hope that sharing mine is of use to others. I am deeply grateful to Dr. Lonsdale and Dr. Marrs for their groundbreaking work in this area and hope to do whatever I can to spread the word about this vital information so that more people can experience full health and happiness in their lives.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This story was published originally on December 14, 2020.












I am very late to the game here and wonder where you are at in your health journey today? It sounds like you may have CIRS (Chronis Inflammatory Response Syndrome). I would suggest looking into the Shoemaker Protocol and finding a practitioner to work with.
Hey Charlotte. I am so sorry for your symptoms.but relate SO much. With your history of eds, I was wondering if you’ve been evaluated for MALS? Im also in Australia. Would love to chat!
I hope you are feeling better. I came across your blog after listening to an interview on YouTube under Nutrition With Judy. Of the 2 interview with Garrett Smith, ND, the ‘Part 2’ covers both of them. Judy is asking about Vitamin A toxicity. Also, Grant Genereux has a blog where he has researched Vitamin A in order to heal himself. Please check out these resources and perhaps you can get more of your health back.
While vitamin A toxicity can be real, Grant Genereux and Garrett Smith, a.k.a. Dr. Google, have taken it to extremes of orthorexia. First, it was supposed to take six months to ‘detoxify’, then a year, then 2, then 7. They avoid all sorts of foods that have NO vitamin A content…just bizarre, and frankly, ironically dangerous.
In Genereux’s case, he was suffering from kidney failure, which explains how he became so toxic. But that doesn’t mean it’s good for anyone else, especially to such extremes.
Hi Charlotte
Here a little brainstorming:
Zimmerman and Reiter have produced a paper about light and subcellular melatonin production in mitochondria. Melatonin seems to be the backup antioxidant per se.
Melatonin is built from serotonine – but not in the case of inflammation especially rooted in the gut, then tryptophane is taken for de-Novo synthesis of Niacin/NMN by the kinurenine pathway.
Niacitol from Pure encapsulation might help with the gut.
Betain (trimethylglicine) Pepsin might help to increase stomach acid and intrinsic factor (needed for B12 resorption)
The right prebiotic might help to increase Akkermansia bacteria (butyrate builders), maybe raw potato starch
Butyrate orally or i.v. might help the gut too. (Butyrate is anti-inflammatory)
Check your genetics about inflammation and check the relation of omega 3-6 and 9
Vitamin A is important for the gut.(fermented cod liver oil )
Check glutathione status and if you have deficiencies in aminos (Glutathione is built from Glycin, Glutamine and Cysteine), Glutamine is important for the gut
Zinc prevents inflammation in the gut.
Chewing very well improves digestion according to Dr. Mayr by at least 50%
(Watch how relaxed cows are chewing:-)
Stool transplantation can improve the microbiome.
The trees heal from the roots – humans from the guts
Exercise at below 1.5 mMol lactate has an antiinflammatory effect.
Fermented Garlic in Honey helps blood flow
Liver Gallbladder support from youngevity has an antiinflammatory effect.
Horse chestnut drops can help when blood vessels are inflamed.
(Infrared light above 760 NM has an effect on nitric oxide release and improved blood circulation., example in study of Zimmerman and Reiter)
Weber medical in Germany produces low level lasers to improve pain.
Inflammation in the gut can lead to systemic inflammation via transmission by the blood.
There is a relatively new term of microscopic colitis, which is not easy to detect.
I know 2 excellent doctors in Germany and Austria (digestion and orthomolecular medicine) let me know if you need the adresses.
Best regards
Benjamin
Hi Charlotte,
Sorry to hear that you have gone through so much. I also was never really well and my health took a turn for the worse about four years ago. I went down a lot of blind alleys but the following really helped: Going low oxalate, the Andrew Cutler Protocol, Thiamine (Thiamine HCl, Benfotiamine and Allithiamine), sublingual B12, cutting out PUFAs (soy, corn, canola etc) and sticking with the saturated fats, iodine and other minerals, and giving up caffeine (Caffeine Blues: Wake Up to the Hidden Dangers of America’s #1 Drug).
I think I probably inherited my B1 deficiency from my mother. Source Naturals has a sublingual B-1 that I have been experimenting with.
I would definitely start the process of lowering oxalates. There is a “Trying Low Oxalates” FaceBook group that I have found to be really helpful. EONutrition on YouTube also has great info on oxalates. You might consider greatly reducing your Vitamin C. It was a huge problem for me and I got a lot of relief once I stopped taking it. Vitamin C causes oxalate formation. https://www.everywomanover29.com/blog/vitamin-c-causes-oxalate-formation-resulting-in-pain-anxiety-and-insomnia-when-there-is-a-defect-in-ascorbic-acid-or-oxalate-metabolism/
I also had that lower right abdominal pain and it’s mostly gone now. It took about 6 months of consistent, high dose, multiform B1 supplementation. It sounds like your deficiency started when you were very young so it might take longer. Build up slowly. Don’t give up. HormonesMatter.com is one of the best sites on the internet keep reading.
Charlotte, interesting to read you also get muscle pain when exercising.
I get lactic acid build up very quickly, mainly in my thighs. I believe it’s oxygen deprivation or lack of mitochondria, forcing lactate to be produced instead.
Have you noticed any benefits in this regard as you exercise a lot?
I took 350mg Allithiamine for 3.5 months and recently dropped to 150mg. It’s interesting to see you went all the way up to 1000mg. I was a bit too worried titrating up so high in fear it would cause imbalances elsewhere and I’ve made huge steps in the last 4 years that i didn’t want to hinder.
I think you should SERIOUSLY look into pyrolluria.
check out a number of articles, each differs slightly in explanation, some easier to understand than other; some more comprehensive than others. Information can seem overwhelming at first because there are a gamut of symptoms, and only a few can apply to any one person.
The key supplements you need are vitamin B6 (the P5P form), Zinc and GLA (evening primrose oil). Need specialty lab for the test–But worth just using these supplements even without testing; if you are pyrolluric, you will notice some changes within few days to week. Can make enormous difference quickly, even with the gut pain.
This is clearly due to energy deficiency and it might be purely genetic or because of a high IQ. It certainly does not sound like diet. If there is a genetic cause in the mitochondria, you may be able to overcome it by continuing with your high dose thiamine because of epigenetics (relatively recent science showing that diet and lifestyle can influence genes). Please do not forget high-dose magnesium, B complex and a multivitamin as well. I agree that I/V would be the best treatment but unfortunately this kind of treatment is still foreign to modern physicians.
Hello Dr Lonsdale,
Thank you so much for your message and your work. I have read your and Dr Marrs’ book in detail and think it is truly groundbreaking.
Would love to know more about what you mean by ” it might be purely genetic or because of a high IQ”? On the latter, do you mean that I am using up a lot of energy? I definitely have a tendency towards perfectionism in all things and over-work, which I’ve been working to reign in this year. My brain often feels like it is full of cogs spinning at a million miles an hour, processing a lot of information and thinking about things from every different angle.
Regarding diet – I have extremely high urinary oxalate as measured in a recent OAT test – almost 4x the upper limit, so have been advised to go on a low oxalate diet, which I started recently and am hoping reduces my gut pain.
Re the thiamine dose – do you think it’s worth staying on 1000mg or increasing? I don’t suppose you know of any doctors who administer IV B1 in Australia?
Many thanks
Charlotte
The brain is the most energy consuming organ in the body. A high IQ is an indicator that the brain has a vigorous function and consumes a proportionate amount of energy. So a high IQ is a risk factor that depends on the quality of nutrition to provide the fuel. If you have not added magnesium you should. It is okay to continue the megadose of thiamine.
Charlotte,
Have you been tested for Celiac Disease? You have many of the symptoms of and concomitant health problems. I found getting my Vitamin D level above 75 ng/m beneficial. At higher levels, Vitamin D helps regulate your immune system and reduces inflammation.
“Gastric Dysmotility and Low Serum Vitamin D Levels in Patients with Gastroparesis”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5089061/
I also found tryptophan helpful.
“Acute tryptophan depletion slows gastric emptying in females”
https://pubmed.ncbi.nlm.nih.gov/15005820/
Hope this helps.
L.
Thanks so much Laurie. I have been tested for coeliac and it came back negative but am definitely sensitive to gluten. It seems like the oxalate might be more of an issue in my case in relation to the gut pain. And yes absolutely – Vitamin D is so crucial hey?! I supplement with a D+K spray sublingually. Hope you’re doing really well and many thanks again.
Thanks for all the super helpful comments everyone. Wondering if anyone here is familiar with oxalates? My levels are super high so I’ve been digging into all the literature recently – particularly the amazing work of Sally Norton – super powerful stuff – which seems to fit my case like a glove: https://sallyknorton.com/interviews-talks/#Overviews. Hope it is of help to others. I’m about to start a low-oxalate protocol (gradually to avoid the dumping syndrome). Will be sure to share how it goes. 🙂
Charlotte,
Thiamine and vitamin B6 deficiencies can make you more susceptible to producing excess oxalates as well. See this youtube video by Elliot Overton who has been a contributor to Hormones Matter.
https://www.youtube.com/watch?v=fFF55stxVIw&t=59s
He also has done an interview with Sally Norton about oxalates. He has a lot of helpful videos on YouTube.
Charlotte! the collagen you are having several times a day is a major source of oxalates. Struggling with oxalate issues myself, I figured out that my occasional bulletproof coffee (with collagen AND raw cacao, both high in oxalates) was causing severe constipation, the opposite effect that most folks experience with their “coffee constitutional”. Though it is an iimportant factor in assisting with metabolizing and detoxing oxalates, thiamine can only take you so far – they are toxins and the spinach/kale smoothie guzzling crowd refuses to believe it. Check out Sally Norton’s and Susan Owen’s work on oxalates.Good luck!
What about fasting under medical supervision? The resulting autophagy apparently can do wonders in healing the gut.
Also, I don’t see your diet as being healthy–certainly not enough calories and nutrients to maintain healing, given the amt of energy you expend each day.
Hey e! thanks so much for your message. You’re absolutely spot on that it’s not enough food – the challenge I have is being able to eat enough with my terribly painful gut. Really trying to find novel ways of getting more food in without debilitating pain and gastroparesis but it’s not an easy one. But committed to find a way through! As for fasting, I do pretty poorly on that and sadly my gut totally shuts down and stops moving, so have been advised not to do it. Even intermittent fasting can do that for me. But as you say, it can do wonders for others! 🙂
okay–
have you explored that you probably have a Potassium deficiency?
super imp for muscles and nerves, and for gut motilty…
we need at least 4700 mg per day—-
Here is a link to an article about vitamin B12 and hypervitaminosis A, which I thought you might find interesting:
https://nutritionrestored.com/2020/07/29/vitamin-b12-folate-folic-acid-depleted-by-vitamin-a/
Awesome thanks so much K.W!
Hey Charlotte!
Sounds like your health journey has been extremely difficult.
Mine wasn’t as bad, but I have had disabling CFS/POTS since I was 16 years old, as well as Clinical Depression/Mania/OCD/GAD and severe menstrual problems, which eventually developed into PCOS. The mental health problems I have recovered from completely, but I am still working on the remaining CFS/POTS symptoms.
Have you ever heard of hypervitaminosis A? Because I now believe that the CFS/POTS and mental health problems that came on so suddenly when I was a teenager were the result of a “poisoning” of vitamin A. Sounds kinda wild, but I sure “felt poisoned” back then…
When I “accidentally” lowered my vitamin A intake 7 years ago (I am 31 years old), my mental health symptoms went away quickly. Once I realized that was the factor (only took 5 years lol—and Grant Genereux figured it out, not me), I stopped eating vitamin A almost completely. Within the first two weeks the gut irritation, constipation, mucus, and other bowel issues I was having went away.
Over the past 2 years, the low vitamin A diet has helped me go from from obese with PCOS, to a normal weight with predictable, regular mensuration! (And I cannot exercise due to my CFS, but I still lost weight easily without caloric restriction.)
Since this summer, I have been working with Dr. Garrett Smith (of Nutrition Restored), who has helped me to supplement minerals in which I was running low. Also, I have been supplementing thiamine since spring, which has improved my energy and stamina and brain fog! ?
When you talk about the “gut burning” it really makes me think you may also be struggling with vitamin A poisoning—vitamin A turns into retinoic acid, and that stuff is nasty! I take activated charcoal to absorb it, as well as soluble fiber, which also absorbs the toxic bile for elimination.
Anyway, Dr. Garrett Smith is the one to talk to about all of this. Grant Genereux has written three free ebooks about hypervitaminosis A as well (he is an engineer, not a “health guru,” and makes no money from his work in nutrition), and has a free forum where people talk about experimenting with his ideas.
Hey K.W!
I’m so sorry to hear that things have been so hard for you too. My heart goes out to you. Good on you for persevering and finding some relief – that’s brilliant!
I will definitely read more about the Vit A – thanks heaps for sharing the info. My doctors say I don’t metabolise Vit A and actually would like me to take the drops, so my situation may be a little different, but very interested to learn more.
Hope your health continues to recover.
Much strength to you!
I recognise lots of this history in myself. My heart goes out to you. One thing I notice is you take ALA. At this point, I’d be inclined towards expecting you are heavy metal toxic. If you were to investigate the Andy Cutler Protocol, it would talk about appropriate use of ALA (low dose on the half life) during “rounds”, followed by rest. Ad hoc use of ALA will mobilise stored mercury, in particular, and increase toxicity and oxidative stress. The Andy Cutler protocol saved my life. Good luck!
ah that is great to know Leon – thank you! I will read up! I am so sorry you’ve battled with many of the same things and hope you are doing really well now.
Dear Charlotte,
I am curious, did the pain in the lower right quadrant disappear? Did you link it to anything?
I have myself experienced this frequently throughout my life, and was always worried that it was the appendix, until I figured out that it was a gut motility issue, basically the valve between the small and the large intestine was not properly functional, it would get blocked in an open position, presumably by the food that was not moving through as it should.
I have been able to reduce the pain quite successfully when it happened, by using a “massage” technique, where you slowly and not too hard press down just below the painful area, and then pull up towards the painful area, so as to cause the gut content to move through in the direction it should, from small intestine into large intestine. There are plenty of videos online about it.
Hey Christine,
Thanks heaps for reaching out.
It hasn’t gone away unfortunately – and has been there since I was about 4 years old. But I’m currently looking into oxalates given how high my levels are and am hopeful that might help.
The massage sounds great too – I have tried that with my masseuse and it sometimes helps.
Hope you are doing well!
Hey! Look into Choline and gastroparesis!! With out choline your nerves can’t signal one another in the gut and then you can’t function at all. Choline is also recommended to people with POTS.
Hey Rachel – thank you so much! Yes taking a bunch of choline both in supplement form (via liposomal Vit C) and pastured organic eggs.
Hi Charlotte,
Wow! Good for you for getting such detailed testing and recognizing thiamine. In your first paragraph, it screamed thiamine deficiency to me, recognizing the symptoms from my own years of suffering too.
My heart goes out to you. I’d love to talk and learn more with you. I too have published my story here on hormones matter and learned a great deal from Lonsdale and Marrs. I too have greatly benefited from lipothiamine, currently taking 8-900 mg along with testing out using hcl form with it to try different avenues of absorption. I’m currently having trouble finding lipothiamine IN STOCK. I was getting 4 bottles monthly but they have been out of stock, unsure why.
So I tried using lipothiamine, hcl form, and ALA if running low on lipothiamine, taking other ttfd forms. I seem to do best on lipothiamine and perhaps I need to up my dose when it returns to stock??
I see your multiple lifetime causative factors as well as genetics, like in my family. The more people I talk to like us, the more I see our life long probability of needing higher doses. Love to talk more with you, so we may share learning experiences. My heart goes out to you at your young age. I’m excited to know you’ve learned so much! It’s a lengthy process of self educatedly self experimenting, for few doctors have much knowledge about dosing. Hopefully, by sharing our stories, we can bring more awareness and studying of THIAMINE. As a nurse, I see the symptoms in so many. Not being an expert myself, I passionately research. ❤️??
Thank you so much for your beautiful message Jane. It would be wonderful to connect and share more of our journeys with one another. Really eager to ensure I can share what I’ve learnt to help others and eager to learn more from all of you. Health is such a complex and challenging thing.
Have you tried a Carnivore diet? Might be worth a 30 day trial. Best wishes for a full recovery.
Hi Ann,
Thanks so much for your message. I haven’t but find that my gut does waaay better when I’m consuming plenty of veggies and fruits. The peristalsis grinds to a halt and my microbiome gets out of whack when I have too little plant matter / too much animal protein.
I guess a sign again that each of us are very individual hey as I know that many people can really struggle with plant foods.
I would absolutely recommend going plant free. I have all the same gut issues and symptoms EDS etc etc and no plants was like a miracle. Just a miracle…
My medical history overlaps a lot with yours. It may be worth trying hydroxocobalamin shots if you haven’t? (Methylcobalamin doesn’t really convert into adenosylcobalamin, and the latter is needed in small amounts for neuropathy. Hydroxocobalamin is totally fine for MTHFR; I’m C677t +/+.)
Awesome suggestion – yes I’ve been really careful to ensure I am taking methylated forms of b12 and the activated B vitamins. I’ve been having methylcobalamin injections and taking it sublingually since finishing the injections. Have you found the b12 to help? I think it has assisted with my nerve/neurological symptoms.
I am COMT (and VDR) and in fact I am supposed to avoid Methylcobalamin and only do Hydroxy/Adenso to avoid the extra methyl groups. Just something to look into and consider!
Additionally, do you supplement B2 with your B1? Something to also look into.