I can remember my anxiety issue starting around 1994, I was driving my then girlfriend and her brother to a concert in St. Louis, MO. I was fine on the way there but as we got closer to the event, I started to feel uneasy, palms were drenched with sweat, my heart beating out of my chest and I felt nauseous. I didn’t go to the concert with them I stayed out in my truck. Every so often I would get out and tell myself I was going in, but that never happened. I have always been the kind of person that has a way out. By that I mean, if I was driving I would have all of these different theories going through my head as to what I would do in a certain situation. The same holds true for being in public places. I would wonder where the exits are and how many are there. I never really thought too much about all this until the middle the to late 90s. I was working as a salesman for my parent’s business and my hands would constantly drip sweat. If I answered the phone the receiver would be wet. I had to wipe my hands on my slacks before shaking someone’s hand. On my honeymoon with my first wife, we were to go and watch the Blue Angels fly, but I just couldn’t force myself to go. We ended up staying at the hotel all day. My mom’s side of the family has a history of depression/anxiety she talked me into going and talking to our family doctor.
The Pill Factory
I explained everything to my doc and he asked the normal questions: have I ever thought of killing myself, was I tired or had felt fatigued throughout the day, how was my social life or did I prefer to stay home? He felt my symptoms were more of anxiety and not depression so he first prescribed Lexapro and told me to let him know if I felt it was working or not. I didn’t like Lexapro, my hands still were sweaty and I just didn’t feel “right”. So after a month or two, my prescription was changed to Prozac. The doctor thought that since my mom was taking it and was doing okay on it, that I should do as well as her. The Prozac didn’t last more than a few weeks. It made me feel “fuzzy” and tired all the time and I felt depressed, which I never felt before. They say the third time is a charm, well in this case it was the beginning of my ongoing issue.
For the third prescription, I was given Effexor. Now, mind you that in most cases, there would be a weaning or purging process to allow time for the other meds to leave my system. That never happened. I was given the Effexor and went home and took it as prescribed. The first night I didn’t seem to have an issue with it. The second night I woke up in a sweat and had what can only be described as an “electrical shock” feeling in my head. I called the doctor’s office as soon as I woke up. I was told to stop taking the Effexor immediately and they would get me in to find something different. As a 20-something back then I just did what I was told to do, it never crossed my mind that I had an adverse reaction to this medication. I got to the doctor’s office the next day and told him what was happening. If I remember correctly, I was told it should subside in a few days. Well, that didn’t happen.
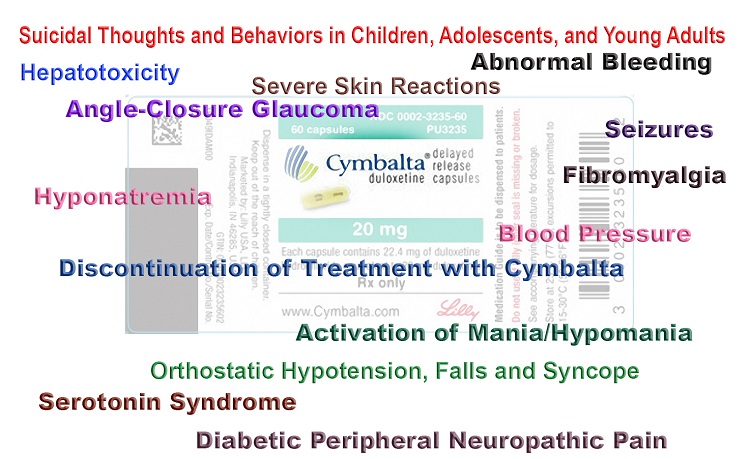
After the Effexor, I talked to my doctor and he said we could try Cymbalta. He said it’s primarily an anti-depressant, but at that point, I was willing to try anything to stop the electrical shock feeling. Within a few days of the Cymbalta being in my system, the feeling was dissipating, and within a few weeks, it was gone. Unless I forgot to take a dose. So here I am, some 20 years down the road taking anxiety medication that I felt I would be off of within a couple of years. Due to the reaction, my system had to the Effexor, I feel as if I’m stuck taking Cymbalta for the rest of my life just so I don’t have to have those shock feelings.
There were times that I have gone to the chiropractor and had a good adjustment and it has alleviated some of the feeling. That tells me that Effexor has managed to mess up my nervous system. I am at present, trying to start the weaning process from the Cymbalta and go with a couple of natural supplements that seem to help. I don’t know how it’s going to go, I’m nervous and scared that because of the 20-plus years of being on an anti-anxiety drug my body is going to do some crazy stuff.
What Now?
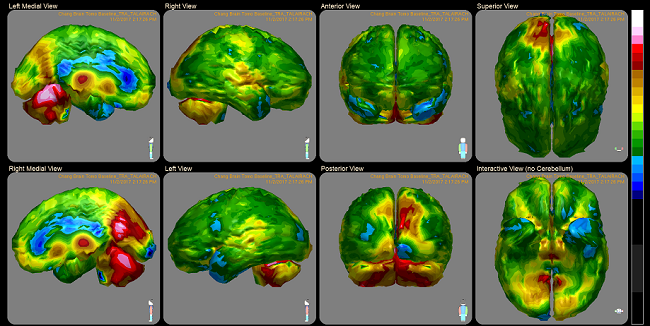
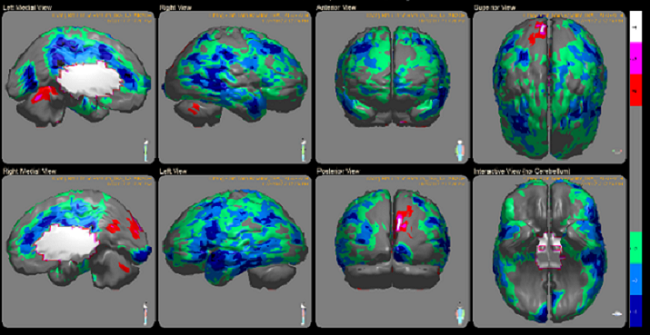
I have read the longer one is on an anti-anxiety or anti-depressant, the more apt you are to sustain long-term neurological damage. Essentially the exact same medications we take to help us are really going to make us sicker, the older we get and the longer we take them.
I haven’t been to the doctor in three years except to have my yearly med check done. I’m ready to stop having to go just for that also, but because of other problems that have arisen in the last few years, I may have to keep going. I have always had better than perfect eyesight, last year at work I noticed it was hard for me to read numbers that I have been reading for years. I went to the eye doc and was told I have an astigmatism, glasses were given and this year I went in for my check because my eyes seemed to be getting worse. Of course, a new prescription was given and I was told that in the next 3 years I will have bifocals.
I have a hard time remembering words when talking to people or trying to tell my boss something that I have told him time and time again. I don’t believe that it is age playing a part in these issues. I think it is the years of being on these medications. I have also noticed that I get angry a lot faster than I ever have, I’ve always had a temper but I have been able to keep it in check quite nicely. Over the last couple of years, I have noticed that it doesn’t take much to anger or upset me. This too is a huge factor for weaning myself, I am the father of five daughters, aged 15 months to 21 years old. I cannot allow this to continue for their sake, and if for nothing else, I need to stop this before it makes me forget who I am.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on January 4, 2018.