My intention with this post is to help inform the general public about a possible cause of various chronic/degenerative illnesses: parasites. I should begin by saying, I am NOT a medical doctor. Although I have much experience working in the healthcare field as an employee of various naturopathic doctors, chiropractors and holistic practitioners and I am a massage therapist and have extensive training in anatomy and pathology, my training and medical experience with parasites occurred AFTER I was diagnosed with endometriosis and used Lupron.
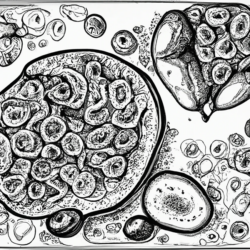
When I say parasites, I am using this term broadly. I am not just talking about worms. I’m also speaking of arthropods, flukes (flatworms), roundworms, pinworms, hookworms, tapeworms, protozoa, fungi, slime molds, mildews, bacteria, spirochetes, mycoplasmas, nanobacteria, etc. Parasites can range in size from microscopic (nanobacteria) to 30 feet long (tape worms). They each have their own life cycle, method of reproduction and can cause damage to multiple organs. In my case, parasites were responsible for my endometriosis and ill-health.
My Struggle with Endometriosis
Since the age of 15, when I finally hit puberty, I experienced crazy irregular periods. I was bleeding every two weeks. Little did I realize when I started my periods that it would be the launch-pad into a life of routine doctor and hospital visits. I had various laparoscopic surgeries for ovarian cysts. I have tested almost every birth control on the market (from the pill to the patch).
No matter what pill I took or what surgery was performed, I wasn’t getting better. Instead, as the years passed, I got progressively worse.
At a young age, I grew accustomed to being sick. I was used to getting my blood drawn and having IV’s inserted (and it usually took 3 pricks to hit a vein because my arms were so “fluffy” from the extra weight I carried). I followed the doctor’s orders, filled my prescriptions, and my parents paid the co-pays thinking they were doing the best of their child.
Everything came to a head in my early twenties, when I was a missionary for my church. My service was cut short due to the symptoms of endometriosis. At that point, doctors had put me on the OrthoEvra patch. It was yet another failed attempt at using birth control to treat my symptoms. Because I was far from my primary doctor, and no one knew what to do with me, I was sent back home.
My primary doctor prescribed narcotics for the chronic pain and referred me to a gynecologist who was well-versed in endometriosis. His opinion, after many diagnostic procedures, was that the endometriosis had spread so much that the only option I had was to try Lupron as an attempt to save my uterus. If it didn’t work, he would do surgery.
I opted for Lupron.
He also informed me he wanted to prescribe Prozac to help with the side effects that come with Lupron. I was already well versed in the side effects of Prozac, and that wasn’t something I wanted to deal with. I politely declined.
I was told it would be a couple of weeks before the Lupron would be available, due to needing pre-approval from my parents’ insurance (since it cost $500/shot at that time). Upon leaving the gyno’s office, I started to grow a wild hair… I decided to make a pit stop to the health food store before I went back home. I bought a bottle of herbs for female hormone balance for $6. It was the best decision of my life.
One week after taking the herbs I noticed that the pain was starting to back off. I was able to ween myself off the pain killers. By the time I was back at the gyno’s office to get my first injection of Lupron, I was already having second thoughts. Why go through with this drug if the herbs are working? I really wish I had listened to my gut in that moment. Once I had my first injection, my life started to turn into my own personal hell.
Hot flashes, pain in my joints, lethargic, constantly hungry, and moody; I was no longer myself. Granted, I wasn’t in pain like before, but the pain was gone when I started the herbs. I couldn’t say Lupron did anything for the endometriosis pain. All I knew is the effect of the drug was worse than I expected. I felt like I aged overnight, and I didn’t know what to do about it.
After two injections, I made the decision to stop using Lupron.
Fast forward a couple of years later, I eventually got married and became a widow before I celebrated my one year anniversary. I fired my medical doctor, filed a complaint with the FDA about Lupron and decided to pave my own path to healing. I was done with playing chem-lab with my body. If a $6 bottle of herbs could make that big of a difference, then what else was out there that I had yet to explore?
Introducing the Practitioner Who Saved My Life
I moved out west to Utah in an attempt to build a new life for myself. Some friends of mine, who also re-located to Utah, informed me about a homeopath that helped them overcome the chronic/degenerative conditions that they experienced. One of them was working for him. He let me know that he spoke to the practitioner about my situation and wanted me to come to the office right away. The practitioner said my problem was an easy one to fix.
Now, I’m sure you can imagine what I thought when I heard someone say endometriosis was “easy to fix”. I didn’t believe it. I wasn’t sure what I was in for, but I figured I had nothing left to lose.
During my visit with him, we didn’t really talk much about endometriosis. Instead he educated me on parasites. He informed me that what I was experiencing was actually the result of parasites invading the uterus and endometrial lining of the uterus. I learned how parasites don’t just live in the digestive tract, they can live anywhere in the body. There are parasites that have their preferred organ to dwell in (like liver flukes – the name says it all). They can inhabit the pancreas, the brain, the lungs, the heart and even the body cavity.
It is very easy to become a host; too easy. The tragic thing about parasites is that they go on living, completely undetected, slowly killing their host by leaving them chronically nutrient deficient, suppressing their immune system, burrowing holes in their organs and slowly eating them alive. The worst of it, the medical community has turned a blind eye to this epidemic and traditional diagnostic exams (stool samples and blood samples) aren’t sufficient enough to detect them.
My new practitioner explained how the uterus is a perfect place for parasites because it is a hollow space, isolated from the digestive tract (thus, it can’t be touched by typical parasite cleanses). He posed the question to me, “Now the cells of the endometrial lining of the uterus are specifically designed for that part of the uterus, and nowhere else in the body. How do you think those cells got outside of the uterus? How did that webbing appear from out of nowhere? Does the body decide it’s going to magically displace cells to wherever the heck it wants to? And if you think about it, why are dogs and cats recommended to get de-wormed on a regular basis to help them stay healthy? Dogs have to take heart worm pills every month. Why do we think we are immune to parasites?” When he posed that question, I began thinking about my childhood.
When I was a kid, I used to play with stray cats that lived in my yard. We also had a dog that lived outside. I remember when I finished playing with them, I never washed my hands (I lived in the country so hygiene wasn’t really enforced in my home). It made sense as to why I would get parasites “down there” because if I had parasite eggs on my hands (from playing with the animals) and I used the bathroom, then the eggs could easily have made their way from my hands to the toilet tissue, to my girl space. Or if I used a tampon without washing my hands beforehand… well, you get the picture. It started to make sense.
At the close of my session with him, I was thankful that fate brought me to his office. I felt completely enlightened on my condition. I felt relief that there was someone out there that had an explanation as to what was going on inside my body. I spent the last of my moving money on my bill at his office (this covered his office fee and remedies). I didn’t regret it one bit.
Recovery from Endometriosis and Uterine Parasites
The protocol he used was very simple. First he used muscle testing (Applied Kinesiology) to check to see what kinds of pathogens were keeping my body sick (for example: parasites, bacteria, fungi, molds, mildews, yeasts, etc.) and recommend herbs and homeopathy to kill it off. Then he would check for weaknesses in various body systems and organs and recommended herbs and homeopathy to make them stronger. The idea behind this is that once you get rid of what is suppressing the immune system, then the body’s natural defense mechanisms kick in and the body is better capable of absorbing nutrients from food. When the body is getting the proper nutrition needed, and no longer robbed by the parasites, then the body can start repairing the damage that was done.
The way I knew this was working was from what came out of me when I went to the bathroom. Granted, he did warn me that I might not see much because typically the worms get broken down during the digestion process. I did see some residuals of worms in my stools. They looked like little orange sticks that resembled skinny shredded carrots. I saw a bunch of black granules that resembled sand. I also saw white pieces that resembled sesame seeds and rice.
Six months of working with him I felt like a new person. I felt a huge shift in my body and my being. The cramping and pain had stopped. I had more energy and stamina. I wasn’t feeling down and depressive. I was hopeful for the future. And now seven years later, I am a health and fitness coach, massage therapist, remarried, a mom of two kids (without any hormone therapy) and living a life that I once dreamed of while lying on the couch, watching Sex In The City high on narcotics. Back then, I didn’t even think something like this was possible.
When I speak with other women, currently enduring the pains of endometriosis, and tell them I’m now symptom free and no longer on medications, they look at me like I’m crazy. I know that I’m probably the first and only person to pass through their life making such a claim. When I speak with other medical doctors about my experience, they are quick to brush it off because I worked with a “quack” (because homeopathy is considered hog-wash, even though it’s existed for hundreds of years and is still widely used in Europe). My new primary doctor (who was also my OB when I was pregnant with my kids) saw the endometriosis battle scars on my uterus when he performed the C-Section for my babies. He too refuses to delve into how I recovered from endometriosis.
It blows my mind every time.
Why Is This Being Ignored? Information about Parasites for Doctors and Holistic Practitioners
The reason why parasites aren’t considered in conventional medicine is because most people in the academic/medical field consider parasites to be a third world problem. Parasites are not solely a third world problem. We live in an age where there are no borders and boundaries. We can travel from one end of the earth to the other in a matter of a few hours. We can experience other cultures and ways of life as long as we hold a passport. Because of this, certain pathologies that were isolated in one region of the world are now easily spread to other areas. Wildlife that was native to one part of the world can suddenly end up in your back yard, disrupting the ecosystem, due to someone smuggling it onto a plane. Even our produce and meats are imported from other countries. Just because something may be a problem in one part of the world doesn’t mean we are immune to it here in the US. Just because one species of animal may be a common host, doesn’t mean we aren’t a possible carrier for it as well (especially if the host animal is part of our diet). So despite our insistence to the contrary, parasites are a problem; one likely causing a myriad of chronic health problems (including Fibromyalgia, Chronic Fatigue Syndrome, Irritable Bowel Syndrome, etc.).
Another reason most physicians don’t consider parasites is because, most of the diagnostic exams available are grossly inadequate for parasite testing. Stool samples are the main diagnostic exam for parasites. If there are parasites in the stools it’s still not an accurate representation of what’s going on inside the rest of the body. Nevertheless, stool samples are a good start, but they are not commonly used in primary care.
If you are a naturopathic doctor, it would be of great benefit to you and your patients to consider adding some form of testing for parasites to your protocol; especially when dealing with patients who struggle with chronic/degenerative illnesses and who are not benefiting from diet and lifestyle changes or conventional medications. If you are a practitioner that wants documentable proof (especially for insurance billing), then prescribe a stool test for your patients to check for parasites. There are various labs that do detailed exams for parasites. You can find them on Google, but here are some labs that offer parasite testing:
- Great Smokies Diagnostic Labs: 1-800-522-4762
- Diagnos-Techs: 1-800-878-3787
- Doctor’s Data: 1-800-323-2784
- Parasitology Center: 1-480-767-2522
Please note, I have no association with these labs. These are provided for informational purposes only. Even though stool samples are considered the gold standard for parasite testing, a better way to test for parasites might be muscle testing. This is the method that was used by the doctor who helped me overcome the parasites that were wreaking havoc on my health. Muscle testing isn’t as widely accepted in the medical field, but that didn’t concern me.
Muscle testing (aka: Kinesiology) is a tool that taps into the innate wisdom of the body and, when used properly, allows the body to “tell” you what is wrong with it. I have had this used several times in my life using various healing modalities that I learned in massage school. I was always pleasantly surprised how accurately those I worked with were able to get to the cause of a problem just by asking very specific questions and allowing the body to respond accordingly. Unfortunately, it is not something that medical insurance will cover, nor a means to get diagnoses for the proper ICD codes for insurance reimbursement. All I know is it was the means to get me to where I am today, and I am forever thankful to the practitioner who was wise enough to learn how to use it properly and put into practice what he preached.
For Those Suffering from Endometriosis, Infertility, PCOS, Chronic Fatigue Syndrome, Fibromyalgia, IBS and Other Similar Illnesses: Get Tested for Parasites
If you are one who earnestly desires healing in your life, then you must be the one to seek it out for yourself. You cannot wait for someone else to hand it to you on a silver platter. It’s a complicated process, but as you can read here it’s not always as complicated as it may seem. The answers are usually much simpler than we imagine.
Do your research. Try new things. If you’re already miserable with how things are now, then it’ll be of great benefit to you to change it up.
Just don’t make the mistake of self-diagnosis. Granted, the herbs helped me very much before I received the Lupron injection, but they weren’t the answer to the problem. They were a band aid. I needed the help of a professional who had experience dealing with this problem to help unravel the tangled web that was my body. Don’t be afraid of bringing up the possibility of parasites to your doctor and ask for testing. If your doctor doesn’t believe you, then find another doctor, preferably a naturopathic/holistic doctor.
You were born to live and enjoy your life. Live it by design, not by default. Don’t let some microscopic organism/illness/diagnosis rob you of that joy!
References for Educational and Research Purposes
If you know of scientific studies connecting parasites to chronic illness, especially endometriosis, please add to the list.
- Here is a medical case study of a woman in India with chronic pelvic pain and ongoing bleeding for two months. Her uterus was removed and upon examination they discovered a cyst on her fallopian tube. Within the cyst was found parasite eggs and a degenerating worm tail. They also acknowledged in the study that the woman had no trace of worm eggs in her stool: http://www.jpgmonline.com/article.asp?issn=0022-3859;year=1984;volume=30;issue=1;spage=51;epage=2;aulast=Shroff
- A question posed on Google Answers about parasites in the uterus/vagina and why diagnosis of them is non-existent (this also references the above link): http://answers.google.com/answers/threadview/id/524377.html
- Another medical case study where the reproductive tracts of women in Africa were infested by parasites from bathing in local rivers and lakes: http://news.ku.dk/all_news/2010/2010.10/parasite_infects/
- A Cure For All Diseases by Hulda Clark, Ph.D., N.D.
- Overcoming Parasites Naturally by Dr. James Overman, N.D.
- Galland L, “Intestinal Protozoan Infestation and Systemic Illness”, in Textbook of Natural Medicine, 3rd Edition, Volume 2, J. Pizzorno and M. Murray, editors, Churchill Livingstone Elsevier, St. Louis, 2005, pp. 655-660.
- Monsters Inside Me, Youtube Channel: https://www.youtube.com/playlist?list=PL85C902E5A8A1D956
- Parasites – Eating Us Alive, A Documentary: https://youtu.be/hBj04H6l9xc
- NOVA: Conquest Of The Parasites: https://youtu.be/f2W4tiM3KQQ