My health has declined over the last few decades, to the point that I am totally disabled and haven’t driven in 10 years. I have severe POTS with high blood pressure while sitting and laying down. Previously, it was low. I am not able to stand up as my heart rate goes too high and I feel as though I’ll pass out. I have coat hanger pain, jaw tension, and headaches daily. I am very irritable and impatient. Emotional outbursts crying spells, depression. I feel like I am a completely different person. I am in survival mode. My body cannot shift out of sympathetic dominance. All of this has developed over the last 20 years; a progressive decline until everything hit the fan.
I thought I had a relatively healthy childhood and into my early 20s. I did have mono in 7th grade. Looking back though, I ate poorly growing up and did a lot of crazy starvation diets. I also consumed a lot of alcohol in my later teens through my early 20s. I stopped drinking in 1994. However in 2006, I started drinking on and off again and the night I had the severe vertigo attack, I had been drinking. Since then I haven’t touched alcohol.
My mom passed away when I was 22 and I had my first child at 23, which was a C-section. At 26, I developed rosacea. This was really my first health problem. At 27, I was divorced (1993). I remarried a year later and had another child at 30 years old. Three months later, I had my gallbladder removed. With all of this, I was still active and healthy with only rosacea that would come and go, but it would get really bad on occasions and was very distressing. This was until 2007, when life stressors, poor diet and illness caught up with me.
Unending Vertigo and the Protracted Decline of Health
I started working again in 2000 after we relocated to Arizona. I was a preschool teacher, a wife, and was raising my two sons. I had a very full schedule. I was always a high achiever. In 2004, I opened my own school with another teacher. Things got even more stressful. In January 2007, I had a very emotional falling out with my father and a couple weeks after that I was diagnosed with viral pharyngitis. Within a couple weeks of this diagnosis, I was thrown out of bed with the worst vertigo you can ever imagine. This went on for three days and I was unable to walk for over two weeks. As things were improving, the dizziness never did go away. I sought out multiple practitioners, including neurologists and audiologists, but none were able to help.
I went back to work but I was never the same, having to deal with constant dizziness and feeling of being off-balance. In October of 2007, I wound up in the ER with a resting heart rate of 160. This had come on out of nowhere over the day and by the evening I was very frightened. They gave me lorazepam and sent me on my way. I continued with the constant dizziness and then the anxiety and panic attacks started. My GP gave me a script for benzodiazepine and offered an anti-depressant. I tried the antidepressant and I had a bad reaction. I felt completely numb. I couldn’t laugh smile or have any sort of reaction. That was after just try half a tablet. I never tried that again.
In 2009, I had an ankle injury and was wearing a boot for most of that year. In October, of that year I ended up having a surgery on it. What was interesting is that I was not experiencing much of the dizziness for most of that year. It wasn’t until a couple months later when I had a sudden onset of the dizziness during my physical therapy session. So the dizziness had come back and the anxiety and panic attacks were getting worse. In September 2010, I basically collapsed at work. It was about four or five days later at home, I experienced a severe shift of my energy. I was severely fatigued and now was experiencing POTS.
Is it Lyme? Maybe. Maybe Not.
November 2010, I was diagnosed with Lyme, however, my test was not conclusive. The Lyme literate doctor said my immune system was so weak that it was hard to get a positive result. He diagnosed me clinically. This set me off on a seven year journey of protocols that included benzodiazepines, two IV chest ports, supplements, herbs, homeopathics, bio-hormones, coffee enemas, detoxification therapies, chelation, IV and oral antibiotics, Flagyl, anti-fungal drugs, and every diet imaginable. You name it I did it. We had spent our life savings and I was still disabled and incredibly ill.
I became addicted to the benzodiazepines that he prescribed. He never told me about how addictive they were. I was on them for three years and they made me so much worse! I tried to come off of them several times. They turned me into a 3 year old. I was so fearful I couldn’t leave my bedroom even to cross the hall into bathroom. Finally, in 2014 I was able to kick the addiction. It took me six months of liquid titration.
As If Things Weren’t Bad Enough: Cancer Too.
Also in 2014, I had a huge fibroid and had a procedure called UFE ( uterine fibroid embolization ) to cut off blood supply so it would shrink. I know now I had severe estrogen dominance.
In 2017, I hit menopause and stopped menstruating. I was using sublingual progesterone at the time. The doctor also had me on hydrocortisone for adrenals and a time-release thyroid supplement. These supplements never helped and only made me worse. I was in such bad shape. I wasn’t sleeping for 3 to 4 days at a time and then when I would sleep it was only couple hours. This sleep regime went on all year.
In May of that year, I woke up one morning and left breast had shrunk significantly overnight!! The doctor I was seeing, had me come in. He physically examined me and felt that it was not anything to worry about. He said that I needed to detoxify my breast because it was probably blocked lymph. He told me to do skin brushing on it. I was in such bad shape that I wanted to believe him but I was so frightened. In October, I saw a different doctor and she said I had to get a biopsy. It was cancer. I did not see an oncologist. I did not have any lymph nodes removed or chemo radiation. I just had a surgeon remove it. I left the rest up to God. At this point, I could not endure anything else mentally or physically. The pathology report indicated the cancer was 98% estrogen driven.
A Dysautonomia Specialist Prescribed More Antibiotics
In 2018, I tried one more doctor. He was an autonomic dysfunction doctor and his protocol was quite simple. It was focused on lowering inflammation in the brain and body and balancing gut bacteria. At this point, I had suffered from chronic constipation for at least 10 years, on top of POTS and all of the other health issues. I was put on fish oil, olive oil, Rifaxamin and Flagyl for the possible SIBO and a vagus nerve stimulator. He told me not to use any other supplements of any kind. He claimed that most all supplements were fraudulent and using them would interfere with progress. I could not finish the Flagyl. I was feeling severely agitated and I thought it was due to the drug. I took most of it though. He assured me that the Rifaxamin was very safe and that they actually have renamed this antibiotic as a eubiotic. I did see my rosacea clear up. I had read some research and trials were they used Rifaxamin for rosacea and had a very positive outcome. So over the last 2 1/2 years I’ve been faithful on this protocol. It seemed like I had periods of time where I was able to stand up longer and do more around my house but I always relapsed. I was using the Rifaxamin on and off as per his direction for 10 days at a time. This year he put me on it indefinitely to use daily. I’ve been on it now for 8 months straight, but in July I started to go downhill very fast. I was having a decent spell able and had been able walk around for a a bit, do some limited chores and even able to be out in the pool, but one night my heart just went crazy and began to race. The vertigo came back too. I have been bedridden again since.
Discovering Thiamine Deficiency
After going back to doing some research, I came upon Dr. Lonsdale and Dr. Marrs’ book Thiamine Deficiency Disease, Dysautonomia, and High Calorie Malnutrition. I am thinking thiamine deficiency could be a piece of my puzzle. After reading one of Dr. Lonsdale’s articles on high B12 correlating with thiamine deficiency, I remembered two of my B12 tests. One in 2014, where it was 2000 and one in 2017 was 1600. The max upper range is 946.
Although my ill health was progressive at first, over time, everything has just become unbearable. I have been bedridden now for 10 years. The POTS symptoms are severe and I think I have the hyperadrenergic POTS. My blood pressure is very high when both sitting and laying and when I stand up, both my blood pressure and heart rate climb. I feel as though I’ll pass out. As I mentioned previously, I also have coat hanger pain, jaw tension, and headaches daily. I am very irritable and impatient. Emotional outbursts crying spells, depression. I feel like I am a completely different person. I am in survival mode. My body cannot shift out of sympathetic dominance. I am hoping to get some direction and advice on using thiamine to possibly help my condition.
Supplements, Medications, and Diet
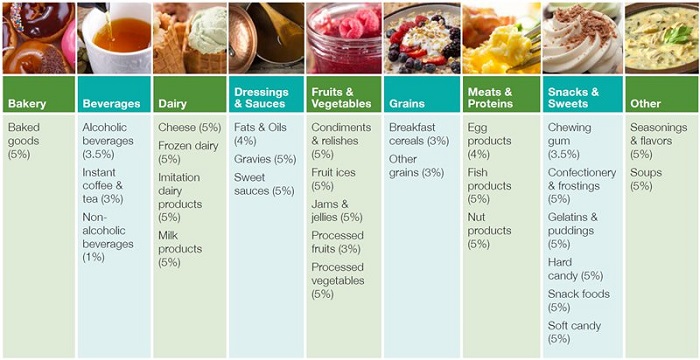
Upon learning about thiamine and mitochondria, I stopped taking the Rifaxamin about two weeks ago. Below is a list of supplements I currently take and some information about my diet.
- Magnesium hydroxide, Magnesium glycinate, 100mg, magnesium citrate, 100mg and some magnesium oxide in an electrolyte drink, in some variation for the past 3 years
- 3000mg daily (6caps) DHA 500 by Now Foods for past 3 years
- Liver capsules 4 daily past 3 months
- Camu Camu powder, a natural Vitamin C, 100-300 mg just started about two weeks ago
- Rice bran 1 tsp before bed started two weeks ago
- Bee pollen 1/2 tsp daily, started 3 months ago
- I follow gluten free diet. I eat beef, chicken, raw liver, raw dairy, raw kefir, cheese, bone broth, some fruit, oatmeal and some vegetables like tomatoes, green beans, onions.
Since learning about thiamine, I have begun using Thiamax but am having a rough time of it. I took my first half dose (50mg) of Thiamax on December 26, 2020 and continued that dose through December 31st. It seemed to increase my fatigue more than my normal, which is already pretty debilitating so I switched to 50mg thiamine HCL on January 1st. By January 3rd, I had a big crash. Hoping to minimize these reactions, on January 4th I took 25 mg thiamine HCL with 12 mg Thiamax in two divided doses. The next evening, however, I rolled over at 2 AM and my heart rate went crazy. I was shaking and went into a panic attack. It took hours to settle down. I haven’t had anything like this in quite a few years and I can’t imagine this would be from the tiny doses of thiamine I’ve been taking. I also took 600mcg of biotin that night at around 6pm. This was for a longstanding fungal infection. The biotin may have contributed to my reaction, but I do not know. I skipped the thiamine and biotin the next day and was able to sleep. I have resumed the thiamine once again and so far, I am tolerating it. I understand that people with chronic health conditions have difficulty adjusting to thiamine and I am trying my best make it through to the other side, but these reactions are difficult to manage. Any input from others who have been through this would be appreciated. I desperately want to recover my health.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by (El Caminante) from Pixabay.
This story was published originally on January 11, 2021.