My experience with hysterectomy and castration (oophorectomy – removal of the ovaries) began in October of 1975, long before information was easily available on the Internet, and in a time when any kind of warning about this surgery was virtually non-existent, and when a doctor’s recommendation was rarely questioned. With that said…
The trauma done to a woman’s life, from hysterectomy and castration, is not something any woman truly wants her friends and acquaintances to know about her. Many women solve this problem by insisting they don’t have any resulting problems. This, in turn, makes those of us who tell the ugly truth appear to be nothing but neurotic kooks.
In all fairness, some of these women may not be intentionally denying the truth. They may simply be uninformed about the numerous potential consequences of this surgery, even though they might be suffering from many of them. During the first 11 years, this was my experience. In spite of the fact that I was going from doctor to doctor, trying to find out “what’s wrong,” it never occurred to me that all of the seemingly unrelated problems I was living with had been caused by this destructive surgery.
Finally, I started learning the truth: I was stuck with this “disabled” existence for the rest of my life. At first, I was overwhelmed with anger at the gynecologist who had told me this surgery was absolutely necessary, without telling me I would be left with numerous, unfixable problems. Eventually, I put the anger on a shelf in my mind, and became determined to warn other women and the men who love them.
Hysterectomy and Castration Consequences: Sounding the Alarm
Fairly quickly, I discovered that my truthful warning was almost always met with indifference, disbelief and sometimes ridicule, even with family and friends. I also learned that this was a common reaction, experienced by many others, who also tried to share truthful warnings. I finally decided that, with rare exceptions, I would share the warning in a written pamphlet, and I would do so anonymously. Maybe this was cowardly of me, but it was the decision I made, partly because I needed to get on with my life, as best I could. I had a business to run, so I didn’t have the time or energy to “go public” or become a crusader.
And then, there was the medical establishment to contend with. They make billions from this surgery and its aftermath. Consequently, they work very hard to keep the general public uninformed, and they’ve done a very good job of it for decades. To make matters worse, any woman who seeks help for problems, following hysterectomy and castration, is told that the problems are all in her head, and she should see a psychiatrist. I know this from my own 11-year experience, as well as hearing it from many other victimized women.
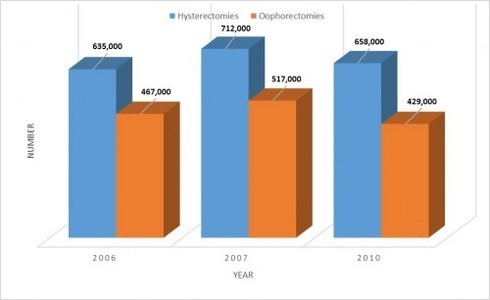
If it were men having problems, after their sex organs had been amputated, they would be taken seriously. Unfortunately, the same respect is not extended to women. When it comes to women, in spite of the fact that we have been anatomically altered and psychologically shattered and sexually neutered, doctors tell us the resulting problems are all in our head. Sadly, this same destructive surgery and the same belittling attitude from doctors afterward still happens to hundreds of thousands of women each and every year. When will it end?
Hopefully, the next Generation Can Step Up
Quite often, I remind myself that it took women over 70 years of pleading and reasoning and persecution and suffering jail time before we were finally granted the right to vote. Some fights for justice and equal treatment take a long time. That’s reality.
Even though this fight must go on, there’s not too much I can do anymore. After 40 years of enduring the damaging consequences of hysterectomy and castration, my physical strength is almost completely gone, to the point that I can barely function. These days, I jokingly describe myself as a physically broken-down old mule with a sparkling personality and a sharp-as-ever mind. It helps if I can laugh about it.
I will never stop caring about the millions of uninformed, unsuspecting women who represent the next potential “crop” of victims, but I don’t have the strength to fight anymore. It’s time for me to leave this struggle in the hands of younger women, and hope they can finally succeed in putting a stop to this legal assault on women.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.