From its title, Mitochondrial Myopathy in Follow-up of a Patient With Chronic Fatigue Syndrome, I doubt anyone would ascertain the importance of this case study, but a quick read of even just the abstract tells an entirely different story. A deeper dive into the full article reveals just how remarkable this case really is. A more appropriate title might have been: Treatment Refractory Chronic Fatigue Syndrome Resolved with Vitamins.
The Case
Here was young man (30 years old) who, six months after surviving infective endocarditis of the native valve that necessitated, not only the use of some pretty powerful antibiotics, but also, an aortic valve replacement and oral anticoagulation therapy, developed profound and unremitting fatigue. Several years and conventional treatments later, physicians considered the mitochondria and the prospect that mitochondrial damage might be behind the fatigue and other symptoms. Mitochondrial testing ensued and upon confirmation, treatment with vitamins, 300mg of thiamine (vitamin B1) and 300mg of riboflavin (vitamin b2) commenced. Within a month, there was significant improvement that was maintained at the five year followup. Effectively, vitamins treated what medicine could not.
The case study is remarkable for a number of reasons, some positive and but most negative. The fact that his physicians went outside of the parameters of conventional, pharmaceutical medicine to the mitochondria is fantastic. Unfortunately, it took three years and multiple, essentially useless medications before looking at the mitochondria and supporting mitochondrial function with nutrients. Had the nutrient requirements to support the mitochondria been considered initially, the patient would not have had to endure a long and progressive decline of health.
Chronic Fatigue and the Mitochondria: An Exercise in Missed Opportunities
Chronic fatigue syndrome (CFS) also called myalgic encephalomyelitis (ME) has become an increasingly common catchall diagnosis for any disease process in which profound and unremitting fatigue is a core component. Symptoms may also include: muscle pain and weakness, autonomic dysfunction, cognitive disturbances and a host of other seemingly unrelated issues. The fatigue is debilitating, persistent and does not resolve with sleep. In this particular case, the patient’s symptoms included:
- longstanding fatigue that did not improve with sleep
- impairment in short-term memory and concentration
- headache behind the eyes and in the back of the head
- post-exertional malaise that lasted more than 24 hours
- dry eyes
- slow digestion with postprandial fullness
- Raynaud’s phenomenon in the coldest winter months
Conventional medicine has no answers for CFS/ME and treatment protocols generally range from psychotropic medications, pain killers, and the like, to cognitive behavioral and exercise treatments. When the symptoms persist and worsen, more medications are piled on. This was the case here.
“He was treated for 1 year with cognitive behavioral therapy, graded exercise therapy, and antidepressants, finding very slight improvement, and the headache did not respond to triptans or ergot alkaloids and responded only partially to nonsteroidal anti-inflammatory drugs.”
Upon each subsequent followup, his symptoms continued to worsen.
“…at the end of the second year, the patient reported feeling more tired, lack of energy, exhausted, with heaviness in the arms and legs, muscle pain, and proximal muscle weakness became more evident throughout the day, and even more after exercise often accompanied by muscle cramps.
About 6 months later, the patient began to feel tingling in the feet, and then in the hands and sometimes burning sensation, along with a sense of restless legs.
In the middle of the third year, these symptoms were more evident and the patient also complained of dry eyes, dry mouth, orthostatic intolerance, intestinal motility disorder with very annoying abdominal bloating, and with persistence of slow digestion with postprandial fullness.”
Routine blood tests were negative across all time points, including a few nutrient tests (vitamin D, folic acid, vitamin B6, and vitamin B12). Unfortunately, no detailed information about the nutrient assays or values were provided.
At three years, a tilt table test was performed and the results showed postural hypotension. At this point, his physicians suspected mitochondrial issues and ordered a muscle biopsy. The biopsy confirmed their suspicions and revealed deficiencies in respiratory complexes 1 and 4. The patient was then started on high dose thiamine and riboflavin, which effectively ameliorated most of his symptoms within a month. The neuropathy persisted and was treated with pregabalin. Five years later, he was still recovered.
Clues for Recognizing Mitochondrial Distress
Reading this case, I am both heartened and frustrated. I am heartened that these physicians continued to pursue options even three years out. Most patients with chronic fatigue languish indefinitely. I am also encouraged that they took the effort to not only followup at five years, but also, to publish the case study. It is infrequent that these cases are published. I am frustrated, however, that it took so long to recognize what should have been obvious immediately, and if not obvious, at least automatically ruled out as part good medical care. In this case, there were significant clues from the onset that mitochondrial issues were present.
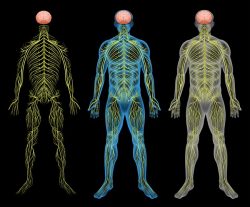
Firstly, fatigue is the cardinal symptom of mitochondrial distress. There is no clearer symptom of mitochondrial distress than profound and unremitting fatigue. The primary responsibility of mitochondria is to produce cellular energy. When they cannot produce sufficient cellular energy, resources are reallocated to survival functions. All other functions become less important and fatigue envelops the person. Fatigue is a mitochondrial survival mechanism. Fatigue tells us that the mitochondria are struggling. It does not tell us why, but it does tell us that there is something causing distress and that there is insufficient energy to resolve the problem.
Secondly, when there are a multitude of seemingly unrelated symptoms, the easiest consideration is mitochondrial distress. Mitochondrial disorders are marked by their variability. Because the mitochondria supply energy and maintain survival functions for the entirety of the organism, for every tissue and organ, when they are distressed, symptoms appear all over the body including the brain and the autonomic system. Again, this is an easy clue to recognize if one is looking. Whenever someone has a wide variety of seemingly disparate and difficult to diagnose symptoms, symptoms that may wax and wane, think mitochondria.
Finally, and perhaps the easiest clue to recognize, this young man underwent a significant trauma just six months prior to the onset of the fatigue. This sort of trauma necessitated not only huge amounts of energy to maintain the requisite inflammatory and immune responses enacted for survival but it required a cocktail of mitochondrially damaging medications as well. Even if he did not have genetic predispositions to mitochondrial disease, the trauma itself, absent proper nutrient support, would initiate mitochondria-damaging cascades. So although he had markers for mitochondrial disease, they were likely to some degree latent, but fully fomented by the trauma of the illness. This was a clue. One that should have initiated some digging. It did not.
Treating Distressed Mitochondria
The most successful treatments for mitochondria, even genetically impaired mitochondria involve supplemented nutrients and dietary modification. The primary objective is to supply maximal energy to organs and tissues and reduce energy losses. This can only be achieved via food and nutrient supplements. Therefore, before beginning a patient on essentially useless and potentially damaging medications (virtually all, if not all medications damage the mitochondria), would not it be more prudent to ascertain if the patient is getting sufficient mitochondrial nutrients and supplement accordingly? It would be. Not only that, if we assessed mitochondrial health and by association nutrient intake and capacity it would save the patient years of suffering and potentially prevent the more permanent symptoms like neuropathy.
Why thiamine and riboflavin? Both are critical to mitochondrial function. Thiamine dependent enzymes sit atop every entry entry point to, and at various junctions throughout, the Krebs (citric acid, tricarboxylic acid) cycle. Without thiamine, everything about the production of cellular energy (ATP), grinds to a halt. Fatigue, is just the tip of the iceberg with insufficient thiamine. Similarly, riboflavin is critical for a number of enzymes within the mitochondria and to the transport of electrons throughout the cycle. Together those two nutrients, plus about 20 others, are necessary for proper mitochondrial function. Without these nutrients, no medication will boost mitochondrial energy production.
For more information about mitochondrial nutrients, see Thiamine Deficiency Disease, Dysautonomia, and High Calorie Malnutrition and/or search mitochondria or thiamine on this blog.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.











What are the about twenty nutrients that are required for proper mitochondrial function?
Dear Dr Marrs, which is the full list of about 20 nutrients, that are essential for mitochondrial function?
Is there an article listing all of them?
Having dealt with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) for 4 years and having gone to 3 conferences at Stanford an one at the NIH on this disease, it is clear that the above article is not about ME/CFS.
Indeed, this patient has mitochondrial issues due to drugs, trauma and nutrient deficiencies, and it is wonderful that these were addressed and he is cured. But, he did not have ME/CFS.
ME/CFS is a multiorgan system disesse that typically affects the nervous system, endocrine, and immune systems, and can be triggered by multiple things. It is complex, and cannot be fixed by giving people nutrients. If eoukd be great if it could be, but saying so trivializes this serious disease.
I see a top ME/CFS specialist, 2 neurologis5s, a hematologist, and 3 functional medicine doctors. My case has challenged each to the limits of their knowledge, and they have consulted other experts to help me. I am not alone.in being this complex, and this help is.paying off. Most are not so lucky.
To date, I have spent over $200,000 on oral and IV nutritional supplemebtts along with testing to identify deficiencies and imbalances. Yes, I’m improving, but the nutrients alone did not do it. It has taken antivirals, antibiotics, naltrexone, immunoglobulins, and drugs for multiple autoimmune problems along the way, as well as therapies like oxygen and light and getting rid of mycotoxins and heavy metals. Many other patients have spinal issues that are a component of their disease which must be addressed for them to improve. Genes play a part as well.
Yes, the article cited and referenced for us by Dr Marrs ecpressly states in its conclusion that the man’s early symptoms were suggestive of CFS but that his later symptoms proved a different conditions. But this doesn’t rule out the possibility of CFS, at least in some cases, involving mitochondrial damage, with possible benefit from a therapy similar to the one outlined here with thiamine and riboflavin.
Hi learner1,
Do you participate in any cfs communities or is there another way i can contact you? Id really like to ask you some questions about the path youve walked and suggestions and or advice
Regards
From your experience, how common is riboflavin deficiency compared to thiamine? It seems that it is as hard or even harder to get enough riboflavin from diet compared to thiamine, but I could be wrong. On the other hand, the issue with thiamine seems to be depletion from body due to excess carbohydrate intake as you mentioned.
Also, with thiamine you treat with lipothiamine (or a better absorbed version compared Thiamine.HCL), how about riboflavin? would an activated version of this work better?
It may be more common than recognized. Thiamine deficiency certainly is. You are correct that diet has a lot to do with both or all nutrient deficiencies, but most medications/vaccinations and environmental chemicals also leach nutrients. As far as thiamine absorption, allithiamine or lipothiamine seem to be best. Although many prefer benfotiamine, it does not appear to cross the blood brain barrier. The HCL formulations are not absorbed as well and thus require a much higher dose. Unfortunately, I don’t know which formulations/brands of riboflavin work best.
Thank you for the explanation Dr. Marrs.
Regards,
MB
Hi Dr Marrs….How can we get Cardiovascular Research Ltd to take the Silicon Dioxide out of their thiamine supplements? Both lipothiamine and allithiamine have it included. Can you suggest a cleaner thiamine supplement? Could one just eat raw garlic and receive the same benefit? If so how many cloves a day?
Thanks and Happy New Year
Why don’t you ask them?
I don’t know that you could get enough via garlic.
I wil 🙂 ….no alternative suggestions ? What do you and Dr Lonsdale take ?
I take allithiamine. I think he uses lipothiamine.
Hi Chandler…..well I called Cardiovascular Research(AF) and asked about removing the Silicon Dioxide from their two thiamine products. I didn’t get a “no we can’t ” I got we can look into it from a product manager. It’s something. ..maybe. Perhaps you and Dr Lonsdale can call them also with a vote for SD removal? 🙂
Are you familiar with really high dose vitamin c therapy?…The Linus Pauling, Robert Cathcart school of thought. They use at the Riodan Clinic in Kansas for various illnesses.. They also use high dose Niacin. I’m wondering what yours and Dr Lonsdale thoughts are on using these two high dose vitamin treatments?
Thanks, Mike
This is to hard for me to understand. I feel like I have hit i brick wall and I am very sad. Until now I have been convinced that I was going to solve this, make us well again. “Fipronil disrupts the insect central nervous system by blocking GABA-gated chloride channels and glutamate-gated chloride (GluCl) channels.” These standard phrases I understand, but I don’t have the language or the education to explore the the rest of it. How it blocks the channels and if there could be any connection to our problems and our extreme need for thiamin.
They say “there is NO specific antidote”. “Monitor for hypotension, dysrhythmias, respiratory depression, and need for endotracheal intubation. Evaluate for hypoglycemia, electrolyte disturbances, and hypoxia.”
In the past I have put fipronil on the dogs and permethrin on the horses, and then I have handled them. We all do well on large doses of thiamin spread out through the day. Are we really using it to calm ourselves down because our GABA-receptors doesn’t work as well any more or do phenylpyrazoles interfere with GABA trough thiamin? The amount of thiamin we have taken in the past three years makes it impossible to think that we suffer from defficiency …
Do you know if phenylpyrazole insecticides (like fipronil) in any way effects thiamin? Is that the way they block GABA?
I do not, but all of the pesticides/herbicides damage the mitochondria by one mechanism or another, so I would suspect that even if there is no direct linkage to thiamine, there are indirect linkages.