I began using the birth control pill in my early 20’s. After 3 years of using the pill, I decided it was time to stop. I didn’t expect the process of coming off birth control to be so harsh. I was wrong. The withdrawal symptoms were unlike anything I had ever felt before. I developed extremely high blood pressure, had tingling and weakness throughout my body, brain fog, and a frightening sense of depersonalization. Not a single doctor could give me any information about what was causing these symptoms, when they would end, or even if they would end. In fact, most of the physicians I saw denied that pill withdrawal was a thing. They said that my symptoms were anxiety and suggested an antidepressant. I knew that couldn’t be the cause of these unique, first-time symptoms. I felt like there was no hope in sight. Through research, I found that I was not alone. There were many women who experienced similar symptoms while withdrawing from hormonal contraceptives, In fact there were thousands of women just like me.
I wrote an article about my full experience coming off the birth control pill and published it on this website, here. Since then, the article has received hundreds of comments from women who developed similar withdrawal symptoms. I decided to make a documentary about hormonal birth control in an effort to help spread awareness, and, to comfort other women who were struggling. Filming a documentary with no crew, no production money, and no experience, will fully test one’s sanity, but I was determined to uncover and document the health effects of hormonal contraceptives. After 4 years of work, I released the documentary entitled, “Hormoneously Alone,” on YouTube. It can be found here. I learned a lot from filming this documentary, and over the next few months, I will be writing a series of articles about the topics discussed in the film as well as other information that I was not able to include.
Ninety-eight percent of the female population will use a hormonal contraceptive in their lifetime. This is likely because it is 99% effective at preventing pregnancy when taken regularly. Using the pill alleviates worry and it is easy to use. In the US alone, this means that about 13 million women use hormonal birth control, with 6 million between the ages of 15-24 and 7 million between the ages of 25-34. I also learned that about 60% of women who have taken the pill have done so for other issues unrelated to pregnancy. Acne, bloating, and cramps are some of the main catalysts for using the pill.
What you may not know, and what I did not know before I began taking the pill, is up to 60% women who use hormonal contraceptives, whether for the prevention of pregnancy or for other reasons, stop taking the pill within 6 months because of side effects. Unfortunately, there is little research on pill withdrawal and why it effects some women and not all. Through my own research, I’ve personally estimated that about 15% of women will experience withdrawal symptoms. This is troubling because these withdrawal symptoms seem to only be recognized by the women who use these products. There are few experts in women’s health who understand pill withdrawal. Most doctors and gynecologists seem unaware of these effects. This leaves most of us struggling to recover on our own.
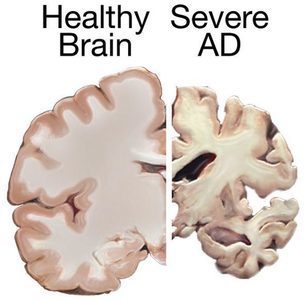
If a significant amount of women use hormonal contraception at some point in their lives, and the side effects both on and off the pill are not well studied, do we really know enough about the well-being of the girls and women who use them? With teenagers especially, are we doing more harm to the developing brain and body when we prescribe artificial hormones for things like acne and painful or irregular periods? Given the large number of girls and women who use the pill, do we as a society, not just as women, understand what we are committing to when we take the pill? From what I experienced and what I learned while producing the documentary, even though the pill has been on the market for over 60 years, we still do not fully understand the implications of using artificial hormones. Over the next few articles, I will be tackling some of these big issues that many women wonder about while on the pill, and off the pill. Hopefully, what I have learned will help others make more informed decisions and feel empowered to know what’s right for their body, and their body only.
Hormoneously Alone – A Birth Control Documentary
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.