In fact, if clinical depression was a guy, all your besties would arrange an epic intervention at The Cheesecake Factory to persuade you to dump his low-life ass. Huddled like quarterbacks over their plates of fried zucchini and fettuccine, they’d each shrill out her impassioned interjection:
“Girl! Get OVER it!”
“Move on!”
“You really just need to get a new relationship and get laid.”
Maybe one friend would generously offer a hard couch in her home for you to crash on. But when depression has put a ring on your finger, you don’t want anybody else’s couch. Dragging your own heavy body every day from your own bed is impossible. Finding an empathetic, capable doctor to treat you is like doing a few hundred rounds of speed dating. And every potential new partner represents just an over-the-counter vitamin- when what you really want is a hardcore-take-with-food- prescribed drug kind of guy. Will this drug be The One? The pill to last a long time and make you enormously happy?
Happy? Oh, no! We all knew THAT word would surface sooner or later. After all, everyone on those anti- depressant commercials looks elated enough to pounce off the picnic blanket, straight up to the clouds. Even radio top 40 threatens listeners to clap happily along. You can’t even zone out to Facebook without getting bombarded by sugary sweet, soul- uplifting platitudes.
“May you go from strength to strength!” That’s a pepper-upper I remember hearing long ago. I suppose it is intended to comfort you if you’re suffering from any number of life’s complicated afflictions. But in the case of clinical depression, does it really apply? I prefer to change it to something more realistic- say, “May you go from the crushing weight of deep despair to sweet mediocre OK-ness.” How can you go from strength to strength when you have no strength to go from anyway? Where’s the journey and near-joy in that?
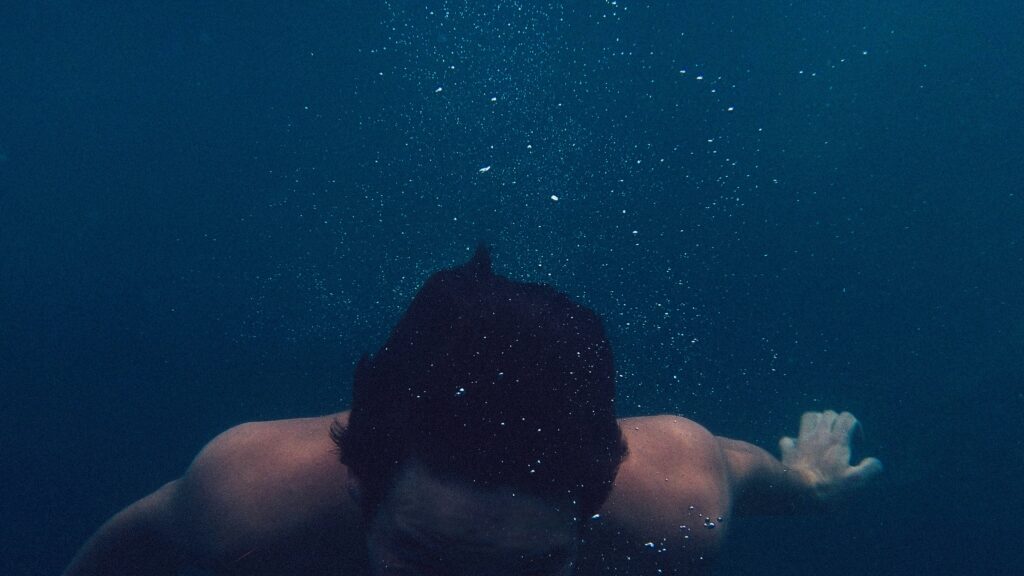
Curious things happen when you hit rock bottom. Since sinking is no longer an option, that only leaves swim. Intuition throws a life preserver for you to catch from the murky depths of nowhere. It talks louder than the sounds of strange inner voices that constantly try to convince you that dying would be best, that “Everyone else would be better off without you.” Once you take that first breath underwater, the fight left in you will rise up again. And in that fight you’ll re-find yourself and start swimming back to clean air and daylight.
Winston Churchill compared the depression he suffered from to a Big Black Dog. I know what he meant. But I’ve also learned I can let Big Depression come, let him bound up to me, even as I marvel at his stunning ferocity from a safe distance. He closes in on me, I open my arms and close my eyes. Bathe in his severe sadness. Feel his full weight. And dance down with him until he whimpers.
I’ve found that in daring to embrace all my emotions, though I’m weak, I’m no wimp. I’ve found that I can survive meeting that Big Dog at the bottom. Then I’m on my way to OK, and being OK is a blessed place to visit. Once there, I open my eyes and take everything in, for I know I won’t be there for long. It’s all good, because now I know I don’t have to fear.
Vulnerability is beautiful; the ebb and flow of our moods is fantastically human and essential. So my friend, don’t fear.
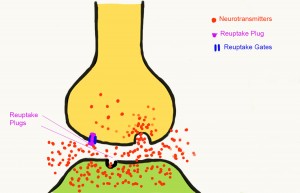
Science is slowly catching up to us. MRI’s and blood biomarkers are pointing out new ways to diagnose depression in the body. Improved methods of treatment and medications that promise to work stronger and longer are coming in the near future. Validation is a needle-prick away.
With all this on our side, you don’t need to always “go from strength to strength”; you can go from weakness to OK. And the only “new relationship” you’ll need to help you overcome your blues will be the One you nurture with yourself.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Volkan Olmez/Unsplash, FAL.
This article was published originally on May 7, 2014.