Studies abound showing how the endogenous estrogens, estradiol mainly, improve memory and other cognitive functions. New research demonstrates there is an even more basic connection between the female reproductive organs – the uterus and ovaries – and the brain. The monthly menstrual cycle may control iron levels in body and also in the brain. Women who have a hysterectomy before reaching natural menopause may be at higher risk of neurodegenerative diseases such as Azheimer’s and Parkinson’s due to the increased peripheral and brain iron levels post hysterectomy.
Iron and Brain Health
Iron is an essential element for health. Both iron deficiency and excess are associated with brain pathology. In the developing brain, too little iron causes neurological impairment with significant cognitive and neuromuscular deficits. As we age, iron accumulation in the brain is also problematic and linked to neurodegenertive disorders. In part because women menstruate, they have naturally lower levels of peripheral (body) iron than men. Researchers believe that the menstrual flushing of excess iron may be in part responsible for delaying the brain iron accumulation that has been linked to early Alzheimer’s and Parkinson’s in men.
In a study published in the journal Neurobiology of Aging, researchers investigated what effect premenopausal hysterectomy had on brain iron levels. From a sample (n = 93) of healthy older, male and female volunteers, ages 47-80 years, researchers used a specialized MRI to image brain iron levels.
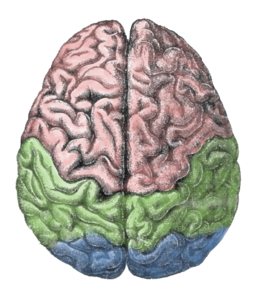
What they found was quite interesting. Women who had hysterectomy before reaching natural menopause had significantly higher iron levels in the white matter of the frontal cortex compared to women who reached menopause naturally. The hysterectomy group, also had higher iron levels in the other brain regions tested but those differences were not large enough to reach statistical significance. Brain iron levels in the hysterectomy group were similar to those of men, who have naturally higher iron levels in the brain and who often succumb to the neurodegenerative diseases at a much earlier age. The researchers speculated that the observed white matter iron accumulation could be a precusor to the grey matter iron accumulation observed in neurodegenerative diseases such as Alzheimer’s and Parkinson’s.
Brain Basics
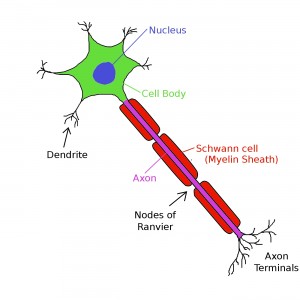
White matter in the brain consists of the oligodendrocytes – a type of cell that forms what is called the myelin sheath. Myelin is the insulation that protects the axons of the neuron (in the brain) or nerve (in the body) to allow rapid conduction or messaging across the brain or to the body. Myelin is like the plastic coating around the electrical wiring in your house. If the coating is too thick, conduction is blocked. If the coating is frayed or too thin, electrical sparks fly everywhere. Iron is a critical component of healthy myelin, too much or too little impairs signal conduction – brain messaging.
Grey matter, on the other hand, is where the unmyelinated portion of neurons – the dendrites and cell bodies – are located. These are brain regions responsible for learning, memory, emotion, sensory perception and motor control. Cells in this part of the brain rely on chemical signaling to translate information. After the dendrite receives and the cell body translates a message, it sends the signal down the myelinated axon to its target. Iron accumulation, either in the white or grey matter would impact brain function. Iron accumulation specifically in the frontal white matter region would impact all higher order cognitive function.
What This Means
The research is still in its early stages. An observed connection between menstrual blood loss and peripheral or brain iron stores though apparent, may not represent the total picture. It is quite likely that hormones associated with reproductive health, altered by the hysterectomy, also play a role in iron regulation. Initial research connecting the hyperandrogenic and metabolically dysregulated state of women with PCOS is associated with increased iron stores, as is general and cancer related inflammation, and genetics. Nevertheless, this study speaks to the critical need for more research about the long-term consequences of hysterectomy. Reproductive hormones regulate more than just reproduction. Removing the organs that synthesize these hormones has health consequences far beyond reproduction. It’s high time we begin addressing this.
If you have had a hysterectomy, be sure to take The Hysterectomy Survey.
Author’s note: I would like to thank David Wiseman Ph.D., M.R.Pharm.S.
Founder, International Adhesions Society (IAS) for introducing me to this exciting new research.