Over half a million hysterectomies are performed each year in the United States. Approximately 60% – 74% of those hysterectomies include removal of the ovaries or ‘castration’. Castration (also referred to as gelding, neutering, fixing, orchiectomy and oophorectomy) is any action, surgical, chemical, or otherwise, by which a male loses the functions of the testicles or a female loses the functions of the ovaries.So there you have it – ugly as it may be. The correct medical term for removal of women’s ovaries is ‘castration’.
Most women do not know that when they agree to removal of their ovaries that they are agreeing to castration. They don’t know because the term castration is never used. They are told they will be undergoing some far-and-away sounding thing called ‘oophorectomy’. Women falsely believe they don’t need their ovaries because their doctors tell them they don’t. Women are purposely led to believe that their ovaries stop producing hormones once they’ve entered menopause anyway. They’re also assured that hormone replacement therapy can replace their own natural hormones. The truth is that there is no artificial hormone of any kind that can replace a woman’s own natural hormones. A woman’s ovaries continue to produce hormones all of her life. There is never a time when a woman doesn’t need her ovaries or the life-sustaining hormones they produce. No woman can give informed consent to ovary removal when she doesn’t understand that she is agreeing to castration. Far too many women are misinformed, uninformed or not informed.
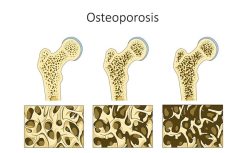
And, it’s not just that women aren’t informed that oophorectomy is castration or that women agree to ovary removal in the first place. I hear from women all the time who tell me that they did not consent to removal of their ovaries, only to wake up from surgery with them missing. It seems doctors routinely take it upon themselves to remove healthy ovaries when they perform hysterectomies for benign diseases. They say it prevents the possibility of ovarian cancer. It should be noted however that the risk of ovarian cancer in women who have no family history of the disease is less than 1%. Meanwhile, removing the ovaries greatly increases the risk of cardiovascular disease (the #1 killer of American women) and accelerates osteoporosis. Removal of ovaries is linked to a variety of diseases and cancers, not to mention mental impairment and sexual dysfunction.
My healthy ovaries were removed without my consent during a routine hysterectomy in 2007 which I’ve previously discussed via my post “Wide Awake: A Hysterectomy Story.” My life has been altered in ways I never knew or understood was even possible. I suppose it’s true that we don’t know what we’ve got until it’s gone. Our ovaries are such a vital part of who we are as women. Yet, it’s not always possible to know this until we are forced to live without them. Ovary removal is not reversible. The devastating consequences last forever. It’s unnecessary trauma at best and forced castration at worst.
Forced castration is considered to be immoral and barbaric according to every country in the world other than Germany and the Czech Republic. More specifically, it’s considered to be immoral and barbaric to surgically castrate convicted sex offenders. Nearly one hundred men have been surgically castrated in the Czech Republic over the past decade. All 94 men had one thing in common: they were sex offenders being punished for heinous crimes. This practice garnered some unwanted attention when the Council of Europe, a leading human rights organization, published a report calling the practice “degrading, invasive, irreversible and mutilating.” Interestingly, the Council of Europe also stated that “even a minor interference with the physical integrity of an individual must be regarded as an interference with the right to respect for private life.”
Indeed, the South Carolina Supreme Court held in State v Brown (1985) that surgical castration is a form of mutilation and therefore considered to be cruel and unusual punishment and illegal under the 8th amendment of the U.S. Constitution. David Fathi, Director of Human Rights Watch’s U.S. program in Washington D.C., contends that surgical castration is “an irreversible punishment and is a fundamental violation of human rights.” Further, he says “Any kind of mutilation is barbaric.” American Bioethicist Arthur Caplan declares “While prisoners are excluded from moral life losing the right to vote, Americans have not reduced them to non-human status.”
If castration of less than a hundred sex offenders is an alarming violation of human rights, what conclusion should we draw from the fact that nearly half a million women are castrated every year in the United States alone. Is it somehow acceptable to reduce women to a non-human status? If it’s considered morally wrong to surgically castrate rapists and child molesters, then why is there no outcry about the castration of millions of innocent women? We simply must begin asking these profoundly important questions.
Quite literally, thousands of women are surgically castrated every single day in hospitals across this country. That works out to be approximately 9 women every 10 minutes. Keep in mind that these women have committed no crime. Innocent and unsuspecting women agree to hysterectomy and wake up castrated. Where exactly is the outrage? What about cruel and unusual punishment being illegal? Does it somehow not apply to women? What about a woman’s right not to be mutilated? Let’s be honest here. If this were happening to men, there would be mutiny in the streets.
It is past time for us to begin talking about the issue of female castration. The ovaries are ‘essential’ parts of a woman’s body. They are part of the fabric of life and so they are integral to the reproductive powers of the body itself. Female castration is simply not ethical in most instances.
I support Hormones MatterTM and their research on hysterectomy. If you have had a hysterectomy, take The Hysterectomy Survey. Your data could save the life of another woman.
My Websites and Social Media
Website: Hysterectomy Consequences
Blog: Hysterectomylies
Twitter: @jiggaz31
Facebook: www.facebook.com/hysterectomyconsequences
A petition to stop unnecessary hysterectomy can be found on the Hormones MatterTM Sign a Petition page: Help Stop Unnecessary Hysterectomy and Castration
Post Script: This article was previously published with the incorrect title: The Ethics of Total Hysterectomy – Female Castration. It is the removal of the ovaries, often with hysterectomy that we contend should be considered female castration. Total hysterectomy does not include the removal of the ovaries. We apologize for the confusion.