I am a healthy 19 year old athlete, or at least I thought I was, until I began having these weird episodes where I will begin sweating, but have the chills too. My heart races and I feel spacey and out of it. It feels as though the blood is just rushing from my head to body. The episodes can last from a few minutes to a few hours and seem to come out of nowhere. The doctors that I have seen cannot find anything wrong with me, but I know this is not normal. I have also had some weird lab results, shown below.
Childhood History
I have no major medical history except for a year of amoxicillin for ear infections and Miralax for constipation as a toddler. Around the age of about 11, I developed facial tics that were resolved with diet change (gluten free) and magnesium.
I have played soccer since the age of 5 years old. I would continuously head the ball, to the point where the parents would jokingly take bets on how many times I would head the ball. Around my sophomore year in high school, I had some back pain and a chiropractor said I have mild scoliosis with a Scheuermann’s presentation. This is basically a benign flattening of the vertebra. He said exercise was important. I changed my mattress, exercised regularly, and the back pain went away. The only other thing that I deal with regularly is altered sleep. I can fall asleep OK but I wake up several times during the night and have trouble falling back asleep.
Acne, Antibiotics, and Accutane and First Episodes
During my senior year in high school I developed severe cystic acne. I tried some dietary interventions, but nothing seemed to help. I did six weeks of doxycycline, which did nothing. I then went on my first round of Accutane for about six months in the spring of 2022. The following fall of 2022, the acne returned. I went back on Accutane for another five months. I discontinued the second round of Accutane at the end of May 2023. Then, one month later, at the end of June, I had my first episode of sweating, chills, heart racing, and feeling of spaciness. It seemed to come out of nowhere. We thought it was viral. A few friends developed Epstein Barr in May and so I thought maybe I had it too, as I was in close contact with them. About a month later, I had another episode and then about two more this past summer. They seemed to be lessening in intensity and duration.
This last fall, we had bloodwork done (Figure 1.). My labs showed that I have exposure to EBV, Lyme and a couple other viruses, which according to the doctor, were not extremely elevated. My albumin, the liver enzyme AST and my progesterone were also high, while my RDW (red cell width) was low at 11.7 (12.2-15.3). My vitamin D was barely above the reference range at 33.3ng/mL (32-100), and strangely my thiamine was super high at 25.0 ng/mL (2.7-10.1) even though I do not supplement. Finally, there was evidence of a lingering respiratory infection Chlamydophila pneumoniae.
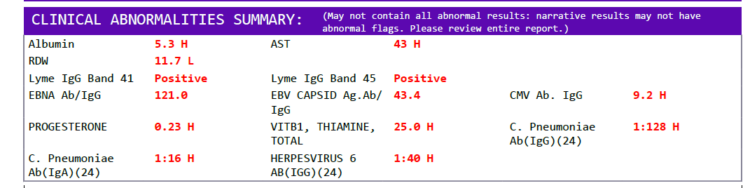
While these numbers were not a concern to the physician, these episodes I have are not normal and so something is going on.
College and More Episodes
Despite all of this, I entered college away from home and felt ok for two months. Then the night before Halloween, out of nowhere, I had another episode. This time it lasted almost two hours. I was sweating, had chills, and my heart was racing. When I feel it coming on, I have to lay down. It feels like the blood is just rushing from my head and body. This time my hands also sort of cramped/seized up, which was scary. I was not doing anything out of the ordinary. I was preparing to go on a road trip. The following night I had another smaller episode. This one didn’t last more than 10 minutes.
Why Is This Happening?
No one seems to know why this is happening. Are the abnormal labs really of no concern? How about the elevated thiamine despite not supplementing? Is there something going on there? Could I possibly have an altered thiamine transporter system or some other genetic defect that makes it difficult for me to use thiamine? Could my symptoms be spinal related? Is my autonomic nervous system altered after coming off two rounds of Accutane? This is very scary to me as a 19 year old. I would like to learn everything I can from you and all the people here sharing their stories. I do not want to get worse.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.