I have never been a fan of Metformin. It seemed too good to be true. Many years ago I had a conversation with a researcher about all of its possible therapeutic indications. His lab was actively pursuing the anti-cancer angle. That should have been a clue that Metformin might be causing more damage than we recognized, but it wasn’t. At that point, I was still enamored with the wonders of pharmacology and hadn’t yet begun my path toward understanding medication adverse reactions. Indeed, it wasn’t until very recently, when a family member began suffering from one of these reactions, that I began my investigation in full. This is what I learned.
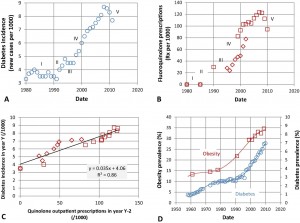
Type 2 Diabetes is Big Business
The global profits from Type 2 diabetes medications rested at a paltry 23 billion dollars in 2011 but are expected to grow to over $45 billion annually by 2020. The market growth is bolstered in large part by the ever-expanding demand for therapeutics like Metformin or Glucophage. Metformin is the first line of treatment and standard of care for insulin resistance across all populations of Type 2 diabetics with over 49 million Americans on Metformin in 2011-2012. It is particularly popular in women’s health with an increasing reliance on Metformin for the metabolic dysfunction observed in women with PCOS, PCOS-related infertility, and even gestational diabetes. Metformin is prescribed so frequently and considered so innocuous that it is sometimes euphemistically referred to as vitamin M.
If we quickly scan the safety research for metformin, there is little immediate evidence suggesting any side effects whatsoever. In fact, in addition to controlling blood sugar by blocking the hepatic glucose dump, this drug is suggested to promote weight loss, increase ovulation in women, (thereby helping achieve pregnancy), and prevent an array of pregnancy complications (everything from miscarriage to gestational diabetes, pre-eclampsia and preterm birth). Metformin is argued to prevent cancer and the neurocognitive declines associated with aging, even aging itself. By all accounts, Metformin is a wonder drug. Why isn’t everyone on Metformin prophylactically? Increasingly, we are.
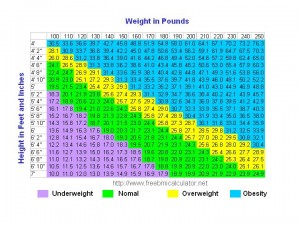
With the increasing rates of obesity and associated metabolic disturbances, drugs that purportedly reduce those indicators are primed for growth. Like the push to expand statin prescription rates from 1 in 4 Americans to perhaps 1 in 3, millions have been spent increasing the therapeutic indications and reach for this medication. Amid all the excitement over this drug, one has to wonder if it isn’t too good to be true. In our exuberance to get something for nothing, to have cake, if you will, have we overlooked the very real risks and side effects associated with Metformin? I think we have.
Metformin and Vitamin B12 Deficiency
As we’ve reported previously, Metformin leaches vitamin B12 and to a lesser degree B9 (folate) from the body. One study found almost 30% of Metformin users are vitamin B12 deficient. For the US alone, that’s almost 15 million people who could be vitamin B12 deficient and likely do not know that they are deficient. What happens when one is vitamin B12 deficient?
Firstly, inflammation increases, along with homocysteine concentrations, which is a very strong and independent risk factor for heart disease (the very same disease Metformin is promoted to prevent). And that is the tip of the iceberg.
Vitamin B12 is involved with a staggering number of physiological functions including DNA, RNA, hormone, lipid, and protein synthesis. Deplete vitamin B12 and a whole host of problems emerge, mostly neurological.
Vitamin B12 is critical for the synthesis of the myelin sheaths around nerve fibers. There is a growing relationship between multiple sclerosis, which involves the disintegration of myelin and brain white matter, and vitamin B12 deficiency. Often the first signs of B12 deficiency are nervous system-related with cognitive disturbances and peripheral neuropathy among the most common.
Additionally, many women have dysregulated hormones connected to vitamin B12 deficiency. In light of the Metformin-mediated vitamin B12 deficiency, one has to wonder if some of the chronic health issues plaguing modern culture are not simply iatrogenic or medication-induced.
Metformin, Pregnancy and Maternal and Fetal Complications
Considering that half the population is female, many of whom are on Metformin and may become pregnant, we must consider the potential effects of Metformin-induced vitamin B12 deficiency during pregnancy. As troubling as the effects of B12 deficiency are on non-pregnant individuals, during pregnancy they can be devastating. Vitamin B12 deficiency during pregnancy leads to an increased incidence of neural tube defects and anencephaly (the neural tube fails to close during gestation). Once thought to be solely related to folate deficiency (vitamin B9) which Metformin also induces, researchers are now finding that B12 has a role in neural tube defects as well.
Scan the internet for Metformin and infertility and you’ll see long lists of fertility centers boasting the benefits of this drug. During pregnancy, the exuberance for vitamin M is palpable, although entirely misplaced. Early reports suggested Metformin would reduce an array of pregnancy complications including gestational diabetes. The data supporting these practices were mixed at best. At worst, however, they were downright incorrect. Metformin, it appears, may evoke the very conditions it was promoted to prevent during pregnancy and then some. Additionally, recent research suggests Metformin alters fetal development and induces long-term metabolic changes in the offspring, likely predisposing the children to Type 2 Diabetes, an epigenetic effect perhaps.
Metformin Inhibits Exercise-Induced Insulin Sensitivity
As if those side effects were not enough to question mass Metformin prescribing practices, it appears that Metformin reduces any gains in insulin sensitivity that normally would be achieved from exercise. I cannot help but wonder if Metformin impairs insulin signaling in general. Cancer research suggests that it might.
According to one study, physical exercise can increase insulin sensitivity by up to 54% in insulin-resistant individuals, unless of course, they are taking Metformin. Metformin abolishes any increased insulin sensitivity gained by exercise. Metformin also reduces peak aerobic capacity, reducing performance and making exercise more difficult. Moreover, despite claims to the contrary, Metformin does not appear to be an especially effective tool for weight loss, netting a reduction of only 5-10 pounds over 4-8 months. Regular exercise and a healthy diet net on average a loss of 5-10 pounds per month for most people and are significantly more effective at reducing diabetes and associated health complications without the potential side effects.
Metformin and Mitochondrial Damage
Perhaps most troubling amongst the Metformin side effects is its ability to severely impair mitochondrial functioning.
Recall from high school biology, the mitochondria are those bean-shaped organelles inside cells that are responsible for cellular respiration or energy production. Through a variety of pathways, the mitochondria provide fuel for cell survival. In addition to cellular energy production, mitochondria control cell apoptosis (death), calcium, copper, and iron homeostasis, and steroidogenesis. In essence, mitochondria perform the key tasks associated with cell survival, and indeed, human survival. Damage the mitochondria and cellular dysfunction or death will occur. Damage sufficient numbers of mitochondrion and chronic, multi-symptom illness arises.
As we have come to learn, many pharmaceuticals, environmental toxicants, and even dietary deficiencies can impair mitochondrial functioning and induce disease processes that are often difficult to diagnose and treat. Metformin is no different. Metformin impairs mitochondrial functioning quite significantly by several mechanisms and, in doing so, sets off a cascading sequence of ill effects.
At the center of metformin’s mitochondrial damage is its effect on the most basic of mitochondrial functions – ATP (cellular energy) production. Metformin reduces mitochondrial ATP production in skeletal muscle by as much as 48%. Sit with that one for a moment, a 48% reduction in cell fuel. Imagine functioning at only half capacity. This would make basic activities difficult at best and exercising to lose weight a very unlikely proposition. Imagine similar reductions in ATP production were observed in the brain or the heart or the GI tract (which, when on Metformin are likely), the types of disturbances we might see become quite clear: neurocognitive decline, psychiatric instability, neuropathy, heart rate, rhythm and blood pressure abnormalities, along with gastrointestinal distress to name but a few. Underlying all of these symptoms, and indeed, all mitochondrial dysfunction is an overwhelming sense of fatigue and malaise.
Metformin Alters Immune Reactivity via the Mitochondria
As I wrote in a previous post:
Some researchers argue that the mitochondria are the danger sensors for host organisms; having evolved over two billion years to identify and communicate signs of danger to the cells within which they reside. The signaling is simple and yet highly refined, involving a series of switches that control cellular energy, and thus, cellular life or death. When danger is present, energy resources are conserved and the immune system fighters are unleashed. When danger is resolved, normal functioning can resume.
If the danger is not resolved and the immune battles must rage on, the mitochondria begin the complicated process of reallocating resources until the battle is won or the decision is made to institute what can only be described as suicide – cell death. Cell death is a normal occurrence in the cell cycle of life. Cells are born and die for all manner of reasons. But when cell death occurs from mitochondrial injury, it is messy, and evokes even broader immune responses, setting a cascade in motion that is difficult to arrest.
Metformin alters this process, first by damaging the mitochondrial ATP factory and reducing energy production capacity and then by inhibiting the signaling cascades that would normally respond to the danger signals. The double hit fundamentally alters immune function and I would suspect predisposes those who take Metformin to more infections and an array of inflammation-based disease processes. More details on this in a subsequent post.
Metformin and the Statins: Beware
The mechanisms through which Metformin derails mitochondrial functioning are complex but likely related to depletion of coQ10, an enzyme involved in what is called the electron transport chain within the mitochondria. CoQ10 also referred to as ubiquinol and ubiquinone, is critical for mitochondrial functioning. Recall from a previous post, that statins, like Lipitor, Crestor and others also deplete coQ10 and from a pharmacological perspective these mechanisms are implicated in the development of atherosclerosis and heart failure.
“statins may be causative in coronary artery calcification and can function as mitochondrial toxins that impair muscle function in the heart and blood vessels through the depletion of coenzyme Q10 and ‘heme A’, and thereby ATP generation.”
CoQ10 depletion is also implicated in the more common statin-induced side effects like muscle pain and weakness and in severe cases, rhabdomyolysis. Since Metformin and statins are regularly co-prescribed, the potential for severely depleted mitochondria and significant side effects is very high. Consider muscle pain and weakness among the first signs of problems.
My Two Cents
When we contrast the reduction in glucose mediated by Metformin with the damage this medication does to the mitochondria and immune signaling, along with its ability to leach vitamin B12, block insulin sensitivity and reduce aerobic capacity, one cannot help but wonder if we are causing more harm than good. Admittedly, obesity and hyperglycemia are growing problems in Western cultures. As we are coming to learn, however, obesity itself is not linked to the diseases processes for which many drugs like statins and Metformin are promoted to protect against – the obesity paradox. Growing evidence suggests that obesity is indicative of mitochondrial dysfunction and chemical exposures which then may provoke impaired insulin sensitivity and hyperglycemia and continued fat storage versus metabolism. If this is true, simply reducing circulating glucose concentrations, in an effort to reduce obesity and the purported health problems associated with obesity, will do nothing to treat the underlying problem.
Insulin resistance and the associated hyperglycemia are environmental and lifestyle-mediated problems that should be reversible with environmental and lifestyle changes. Having said that, those lifestyle and dietary changes will fail unless we consider the underlying mitochondrial damage initiated by dietary choices, pharmaceuticals, and other environmental exposures. For that, we must dig deeper into mitochondrial functioning and correct what we can.
I believe obesity and hyperglycemia are symptoms of damaged and dysfunctional mitochondria, partly mediated by lifestyle, partly iatrogenic (pharmaceutically induced), and likely epigenetic. If we are to solve the ‘obesity’ problem and prevent the damage mediated by hyperglycemia, we have to address these variables. Failing to do so serves no one except those who profit from our continued ill-health.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.