Introduction
In 1958, Dr. Abram Hoffer (MD) discovered what he termed the “mauve factor” in urine of psychiatric patients. This mauve factor was later falsely identified as kryptopyrrole, but was then correctly recognized as hydroxy-hemopyrrolin-2-one (HPL). This disorder is commonly known as Pyroluria, but the accurate designation is Hemopyrrollactamuria (HPU).
Dr. Hoffer observed that recovery from acute schizophrenia was associated with disappearance of HPL from urine. Similarly, reappearance of symptoms coincided of appearance of kryptopyrroles (or HPL) in urine of patients. Later it was found that large doses of zinc and vitamin B6 suppressed HPL and substantially reduced symptoms for many psychiatric disorders. This is because HPL binds zinc and b6, which results in patients losing large amounts of these essential compounds in the urine. High HPL patients were also found to have low biotin, and manganese. However, loss of zinc and b6 seemed to be the most significant in terms of symptoms.
Zinc is an essential mineral required for numerous biochemical processes, including DNA and immune system regulation. Zinc stores in the body are relatively 60%, 30%, and ~5% in muscle, bone, and skin respectively. In circulation, 80% of the zinc is contained within erythrocytes (red blood cells “RBC”).
Symptoms associated with high urine HPL include:
- Anxiety and withdrawal
- Paranoia and hallucinations
- White spots on nails
- Depression, and explosive anger
- Fatigue
- Insomnia
- Morning nausea
- Gluten intolerance and allergies to food or environment
- B6-responsive anemia
- Weak immune system
- Reduced hair on head, eyebrows, eyelashes, and arms
- Poor dream recall
- Stretch marks
- Skin appears paper thin
- Light, sound, and odor intolerance
- Cold hands or feet
- Hypoglycemia and glucose intolerance
- Tendency to being an addict (alcohol, drugs)
As seen above, many of these symptoms are associated with frank zinc or B6 deficiency. On the other hand, along with other neurological disorders, it was shown that the probability of finding high HPL in psychiatric patients is very high:
- Schizophrenia (acute), 59-80%
- Schizophrenia (chronic), 40-50%
- Manic depression, 47-50%
- Depression, non-schizophrenic, 12-46%
- ADHD, 40-47%
- Dr. Klinghardt has found that 80% of Lyme disease patients have elevated HPL
Case History
This is a male in his 30s who suffered from fatigue, hair loss (crown), and notable reduction of hair along his body. The patient’s history showed a history of teenage social anxiety, and depression. The patient presented with nails containing white spots and vertical ridges. Cold hands and feet have been present for “years”. The patient had prominent shoulder stretch marks that appeared in his early 20’s when he had built muscle “very fast”. The stretch marks never went away. In addition, there was a complaint about joint and substantial neck pain ongoing for few years. Other symptoms include: mild POTS, nausea, and muscle pain.
Social history questionnaire showed that the patient is typically withdrawn with few (early years) to “zero friends’ as he turned to his 30’s. He never liked social events and would take every opportunity to not go, or at least “escape” early from events. The patient complained of low libido, exercise intolerance, and inability to build muscle compared to his early 20’s. The patient also indicated that these symptoms precipitated substantially during a high stress period in 2015.
The patient claimed that he performed plenty of laboratory analyses with several medical practitioners and tried many supplements and diet regimens. Unfortunately, he had minimal success with most of the treatments. He also attempted using zinc picolinate (about 15 mg of elemental zinc) along with B vitamins from time to time, but did not notice major differences.
Family history shows that his younger brother was diagnosed with paranoid schizophrenia along with history of depression in another family member. Interestingly, his brother’s medical provider tested him for minerals utilizing RBC and serum assays. All results came normal except for below range RBC zinc, but with normal serum zinc.
Early Case Results
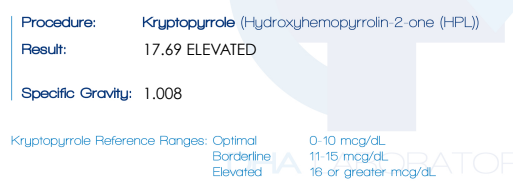
In 2016, the patient was instructed to perform HPL analysis from his morning urine at DHA laboratories. Results confirmed elevated HPL at 17.69 mcg/dL.
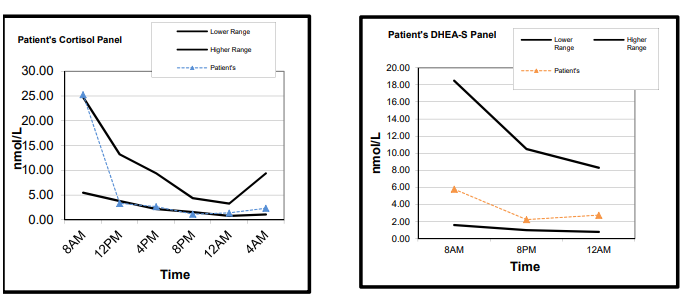
Based on these results the patient was asked to perform RBC zinc analysis, but there was noncompliance and no protocol was initiated. During the following years, the patient saw several physicians who performed numerous blood tests including (CBCs, CMPs, blood/saliva steroid and thyroid hormones, Lyme, minerals, and several other tests such as genetics). His test reports showed no remarkable findings other than consistent below range blood/saliva DHEA-S. Morning cortisol levels were normal in blood but there were signs of adrenal insufficiency in saliva evaluation. The patient was screened negative for anti-adrenal antibodies (screen for autoimmune Addison’s disease).
Interestingly, he had performed copper analysis around 2016 as he believed he was low in copper (he was told that his hair copper was below range). His plasma and RBC copper, as well as ceruloplasmin levels were unremarkable. The patient mentioned that supplementing with 4 mg of copper glycinate gave him vivid dreams but that he became insomniac and agitated after several days on copper.

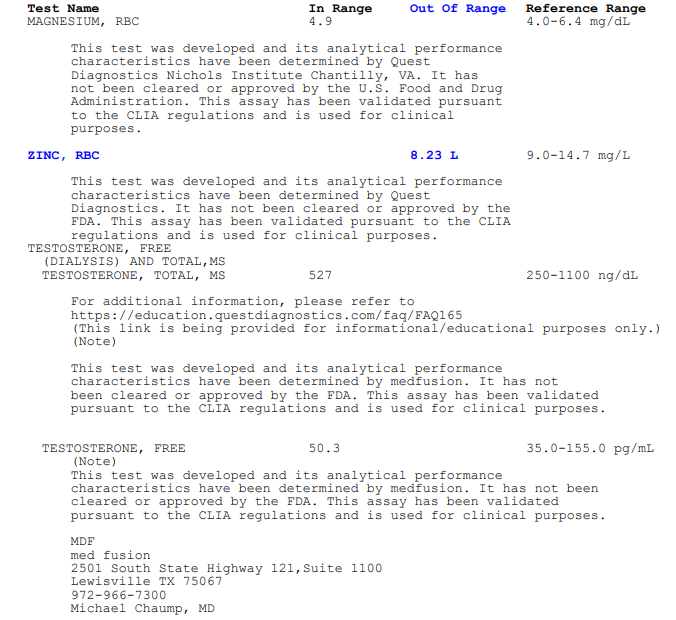
Diagnosis of Zinc Deficiency
The patient recently came back (April, 2023) and asked to revisit “the pyroluria hypothesis”. Because of issues with libido, hair loss, other zinc deficiency related symptoms, and presence of zinc-depleting substances (HPL), the patient was asked to work with his physician regarding performing specific blood assessments. Results showed low zinc RBC values, and sub-optimal free Testosterone. It is important to note here that the patient actually initiated lower dose zinc supplementation (7-15 mg) for 8 months prior to these results. In fact, he had taken 7.5 mg of liquid zinc the night prior to these results. Therefore, zinc deficiency was most likely worse than what is observed here. It is also worth noting that magnesium RBC levels were sub-optimal, but within normal range. The patient claimed that he has been supplementing with 200-400 mg of magnesium glycinate for over a year.
Current Case Results and Treatment
The patient immediately commenced on high-dose zinc regimen along with B-complex. He was instructed to take 60-80 mg of zinc (as zinc glycinate) for two months, and to increase the dose by 20 mg if he experienced any stressful event (exercise or mental stress). The patient was asked to continue using magnesium supplements and to consider manganese supplementation if his physician was willing to test and treat. Note that manganese is different from magnesium.
Within six days the patient started noticing the following bodily changes
- Substantial deepening and strengthening of his voice.
- New observable hair growth in the right arm, followed by left arm a week later. The growth included new hairs and longer hair. This is significant as the patient complained of slow hair growth all over the body with the arms having no hair prior to treatment.
- Significant increase in libido.
- “deeper” dreams.
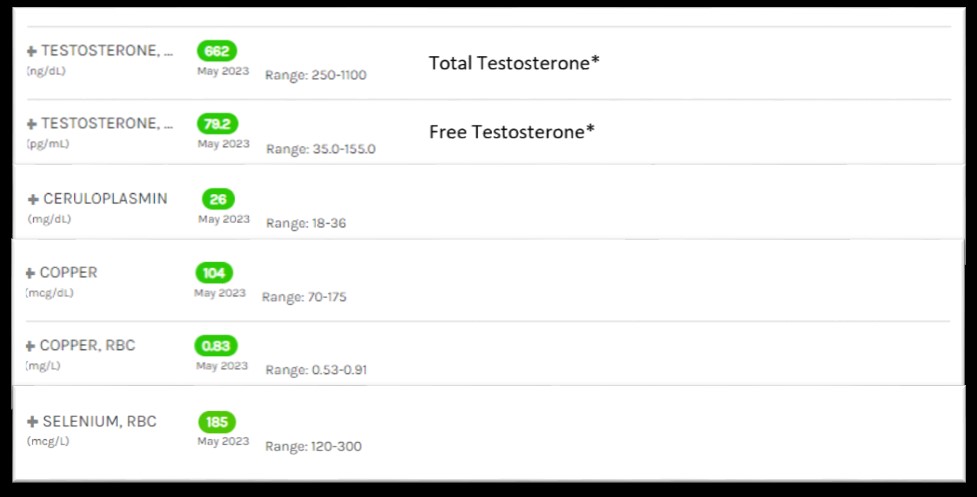
The changes continued to positively increase one month into high-dose zinc treatment (i.e., hair on arms is longer with new baby hairs coming out, hair on head thicker and longer). At this point the patient was asked to reevaluate blood markers for testosterone, but also for copper to make sure that it was ok (long term high dose zinc can substantially deplete copper levels).
As seen below, within a month, total testosterone levels increased by 135. Free testosterone increased by approximately 29. These are substantial changes given that the only major difference in treatment was high dose bio-available zinc glycinate. Importantly, markers of copper are all within range, and look better (higher levels) than his previous report (see above). Nevertheless, copper must be monitored continuously during this type of treatment. For this reason, the patient was asked to begin copper treatment (3-6 mg) two months into treatment. Future blood work for this patient will include zinc RBC levels to confirm that values are approaching mid-high normal range. Because of history of ligament and joint pain, the patient was advised to perform intracellular evaluation for levels of manganese, a mineral that is commonly low in HPU patients. Next, the patient’s selenium levels were near the mid normal range. Therefore, the patient exhibited a seemingly targeted deficiency that did not substantially affect other minerals tested.
Testing For Zinc: Serum Versus Intracellular/RBC
Accurate assessment of total body zinc status is difficult to attain. Measurement of zinc using plasma/serum is the more simple approach but unfortunately these results can be influenced by factors other than just total body zinc stores. For example, there is a plasma diurnal variation for zinc, with a 10 am peak. Plasma/serum levels, like many other compounds, are heavily influenced by recent dietary intake. In addition, individuals with hypoalbuminemia have reduced serum zinc levels. Other disease processes can also affect plasma/serum zinc, causing non-concordance with what is in tissues.
There are strong reports in the literature regarding the discrepancy, or inaccuracy of plasma/serum zinc assessment. For example, this report shows a case of zinc deficiency evinced by clinical symptomology, contradicted by serum zinc levels (normal). Symptoms rapidly improved in this patient after correction with 3 mg/kg/day of elemental zinc. Therefore, serum zinc levels may be misleading unless one has a genetic zinc transporter deficiency (acrodermatitis enteropathica), or a marked chronic deficiency. Even so, a deficiency may still not show in plasma, as observed in one reported case. Plasma levels for nutrients are not going to be in equilibrium with tissue levels in many cases – nor do we expect them to be due the dynamic flux between tissues.
Another example, can be observed here with our patient’s brother who had low zinc RBC but normal serum zinc. Poor correlation between these different tests has been previously reported. Overall, RBC-zinc certainly is better advised in assessing total zinc body stores. Performing plasma/serum zinc levels may in some patients give a false negative result. The same applies to other minerals such as magnesium, as you would find plenty of patients with normal serum magnesium, yet RBC levels are borderline low-normal, or below range.
Conclusion
HPU is a syndrome that results and mental and physical symptoms, many of which resemble symptoms of zinc and vitamin b6 deficiency. The patient presented with current and historical clinical symptomology that agrees with typical patients of krytptopyrroluria. In addition, the patient’s sibling who was diagnosed with schizophrenia, was also observed to have a severe zinc deficiency but normal intracellular levels of other minerals, including copper.
Interestingly, there are some who do not agree that there is a correlation between HPL levels and psychiatric illness. In contrast to these reports, this case amongst others, confirms that some individuals with elevated urinary HPL are highly susceptible to specific nutrient depletion; in this case, zinc. The evidence for this is shown by the low zinc levels, while other minerals were within range (magnesium, copper, and selenium). It is important to reiterate that the patient had already been on small amounts of zinc supplementation for months prior to testing. We also assume that RBC zinc level, although more accurate, is likely a small reflection of total zinc body stores which could be much lower. One should also not shy away from treating HPU patients with copper, as it is also an important mineral that can induce a host of issues if deficient. The reason this patient reacted negatively to copper is likely due to the substantial imbalance between zinc and copper, as demonstrated by his test results. Nevertheless, treatment for all minerals must be calculated and performed appropriately to prevent unnecessary side effects.
It is unclear what precipitated the patient’s symptoms of physical illness. In other words, was it HPU that reduced his zinc levels and contributed to long term chronic symptoms? Or was it stress from some sort of infection that increased HPL in his system? The patient mentioned that he was not diagnosed with any chronic illnesses but that he lived in an apartment with mold for two years, though he never felt physically ill during that time. The patient did undergo severe family and school stressful events prior to his illness. Overall, this case demonstrates the importance of laboratory testing prior to treatment. Of paramount importance is the appropriate dose for treatment, as observed in this case.
Acknowledgment
I would like to thank the patient presented here who has agreed to have his case anonymously presented to spread more awareness about HPU and the importance of zinc.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.












Dr. Bilal
I appreciate you publishing this pyroluria case here and would love to see this and other pyroluria cases published in the mainstream research to further spread more awareness about HPU and the importance of zinc, vitamin B6 and other nutrients that are invaluable in cases like this.
I appreciate that this case “confirms that some individuals with elevated urinary HPL are highly susceptible to specific nutrient depletion; in this case, zinc.” I see a large number of pyroluria cases in my clinical work and can confirm this from my clinical experience too.
I’ll also add that I do see many false negatives on urinary HPL tests and yet many individuals score high on the pyroluria symptoms questionnaire and see symptom resolution with zinc, vitamin B6, evening primrose oil (which enhances zinc absorption) and other supporting nutrients.
I have pyroluria myself, score high on the symptoms questionnaire, do exceptionally well on the nutrient protocol and have had 2 urinary HPL tests show different results – one positive and one negative. These were a few years apart and I was not supplementing before either test.
Dear Trudy,
Thank you, I appreciate your input. Your work on pyroluria is very valuable to physicians, scientists, and patients.
I completely agree with “many false negatives on urinary HPL tests and yet many individuals score high on the pyroluria symptoms”. Like with other metabolites, the concentration of HPL can vacillate in an individual due to biological variations. Therefore, a person may get evaluated (urine in this case) when it is at a lower concentration than the average for that individual. This means that testing at least a couple of times (if it is not elevated, but symptoms indicate) can be helpful.