There are just three days left for the Kickstarter campaign launched by Ricki Lake and Abby Epstein to raise the $100,000 needed to make their next documentary. Inspired by the provocative 2013 book Sweetening the Pill: Or How We Got Hooked on Hormonal Birth Control by Holly Grigg-Spall, Sweetening the Pill, the documentary, aims to fairly critique hormonal birth control and raise awareness of non-hormonal alternatives. Lake and Epstein hope to do for birth control what their acclaimed documentary The Business of Being Born did for birth, get us thinking beyond a one-size-fits-all approach. Currently for contraception, that one-size approach is all about synthetic hormones packaged as—what are now being called—modern contraceptive methods.
Will this film ever get made? I bloody well hope so, and so should the thousands upon thousands of women who have experienced side effects associated with hormonal contraception, from those considered a mere nuisance, to adverse experiences that impair quality of life, to those that threaten a woman’s life itself.
I am not an alarmist, although I do believe that young women dying, however rarely, because they are using hormonal contraception is an unacceptable outcome, especially when safer hormonal and non-hormonal alternatives are available. Women’s health and safety absolutely matter to me, but I want this film to be made so that issues I have been advocating about for 30 years will finally get an accessible, comprehensive public airing.
With that said, here are five take-aways for viewers that I am expecting from the documentary Sweetening the Pill:
1) Hormonal birth control does not, has never, and will never regulate or normalize periods.
There is a false belief held by girls and women of all ages that problem periods are regulated or fixed by taking the Pill. Periods on the Pill are shorter and lighter because they are not real periods. Lara Briden, ND, author of Period Repair Manual: Natural Treatment for Better Hormones and Better Periods, sets the record straight in this June 3rd piece for Hormones Matter: Pill Bleeds are not Periods.
2) Contrary to what women are constantly being told, there are health benefits to consistent ovulatory menstrual cycles. By suppressing ovulation and normal menstrual cycle function we are, over time, depriving ourselves of these benefits.
You won’t get this information from your gynecologist, but you will from endocrinologist Dr. Jerilynn C. Prior, scientific director of The Centre for Menstrual Cycle Research at the University of British Columbia. Prior has over 40 years experience researching the very thing that all hormonal contraception disrupts: ovulation and normal menstrual cycle function. She has written a series of papers on the Preventive Powers of Ovulation and Progesterone that explain the impact of ovulation on our bone, breast and heart health. It is not “incessant menstruation” that’s bad for women’s health, as many OBGYNs would have us believe, but ovulatory disturbances. As I wrote once in a letter to Ms. Magazine challenging the assertion that suppressing ovulation and menstruation is good for our health: “Ask not what those cycle-stopping pills will do to you, but what a healthy ovulatory menstrual cycle can do for you.”
3) The pill should NOT be the standard-of-care treatment for being a girl.
In the foreword I wrote for Grigg-Spall’s book, I noted that: “Prescribing the pill, or other forms of hormonal contraception, has become, in the minds of most health-care providers, the ‘standard of care’ for being a girl.” It’s being used to treat every manner of menstrual cycle problem—irregularity, heavy bleeding, painful periods—associated with the maturation process of an adolescent’s reproductive system. The only sure thing these drugs will do is interrupt this maturation process. Alternative treatments for these problems can be found in the adolescence section on the CeMCOR website. On June 11, 2015, Twitter menstrual cycle advocate Kylie Matthews (@AuntFlo_28) Tweeted me this: “would you believe my 11 year old’s pediatrician already ‘recommended’ I put her on the pill? Of course I know better!” I expect the STP documentary to make sure all mothers know better.
4) Fertility Awareness Methods (FAM) of birth control, taught by skilled educators and enhanced with new technology, qualify as modern contraception.
The mainstream sexual and reproductive health community’s dismissiveness of fertility awareness based methods of birth control and its frustration with women who use or want to use them, must stop. In a previous Hormones Matter piece, I said that women who can’t, won’t, or don’t want to use drug- and devise-based birth control, have the same right to information, support and services as women who are willing and able to use hormonal birth control. Failure of the SRH community to adequately meet the needs of these women is contributing to unplanned pregnancies. But they aren’t the only show in town anymore, and women are seeking out alternative health-care providers, fertility awareness educators, and technological FAM support in droves. The roster of Justisse-trained Holistic Reproductive Health Practitioners is growing world-wide; women can readily access the services of HRHPs like Amy Sedgwick at redtentsisters.com and Ashley Ross at Conscious Birth Control. Tech companies like Kindara and Ovatemp are introducing thousands of women to the scientific principles that underpin fertility awareness methods that are as effective as the Pill at preventing pregnancy. I expect Lake and Epstein’s documentary to leave viewers fully informed as to how women can access the resources and experts they need to learn and use FAM effectively and confidently. If FAM is hot, and it is, then it’s modern contraception.
5) Body literacy, understanding how our bodies work and how hormonal contraception works, must precede birth control decision-making.
Girls deserve to grow up body literate. They must understand how their bodies work and how a normal menstrual cycle unfolds. They must be encouraged to develop a personal relationship with their bodies before they start making decisions, or have decisions made for them, on how to manage their cycles and their fertility. This is a tall order, but if the wave of 20- and 30-something women who are quickly acquiring this foundational knowledge is any indication, it just could be that the next generation of girls will grow up with the life skill of body literacy. They will understand how their sexual, reproductive and general health and well-being are connected to their menstrual cycles. Body literacy supports, if not compels, our fully informed participation in health-care decision making. This is the message I expect Sweetening the Pill to deliver.
So, back to the beginning. There are just three days left to become a backer of Sweetening the Pill, to support the making of a documentary that has the power to change the way we think about our bodies, our health and our birth control. There will always be a place for hormonal contraception, and that’s a good thing. But women need more and better options. We need to know that we don’t need to take it at all if that’s our preference, and that if we do, we don’t need to take it, and probably shouldn’t, for more than a few years of our reproductive lives.
Sweetening the Pill is about the future. Will you be a part of it? To echo my conclusion of the book’s foreword: This film will offer a new perspective on the Pill and its influence on our bodies and our lives, as well as evidence that affirms and confirms we make sacrifices—large and small—to live under its influence. It will remain for viewers to decide what to do about it.
Sweetening the Pill, the Documentary
About the author: Laura Wershler, B.Sc., is a veteran pro-choice sexual and reproductive health advocate and women’s health critic who has worked for or volunteered with Planned-Parenthood-affiliated organizations in Canada since 1986. Laura graduated with a Certificate in Journalism from Mount Royal University in 2011. She has contributed columns on women’s health to Troymedia.com and blogs regularly for re:Cycling, the blog of the Society for Menstrual Cycle Research. Follow her on Twitter @laurawershler.
Participate in Research about Oral Contraceptives
Hormones Matter is conducting an ongoing, online survey of oral contraceptive side effects. If you have ever used oral contraceptives, you are eligible to participate. The survey takes 10-15 minutes and is anonymous. Take the oral contraceptives survey today.
Hormones Matter conducts other crowdsourced surveys on medication reactions. To take one of our other surveys, click here.
If you’d like to share your health story contact us here.
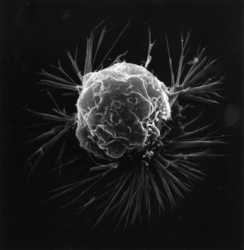
Real Risk Study: Birth Control and Blood Clots
Lucine Health Sciences and Hormones Matter are conducting research to investigate the relationship between hormonal birth control and blood clots. If you or a loved one have suffered from a blood clot while using hormonal birth control, please consider participating. We are also looking for participants who have been using hormonal birth control for at least one year and have NOT had a blood clot, as well as women who have NEVER used hormonal birth control. For more information or to participate, click here.