When I had a stroke at age 28, my doctors did some tests and found that I have a fairly common clotting disorder called Factor V Leiden. They told me that this, combined with birth control pills, are what caused me to have the cerebral venous thrombosis (stroke). It didn’t occur to me then to ask what Factor V Leiden actually was. Or to ask why I hadn’t been testing for inherited clotting disorders before I was put on medication that increased my risk for blood clots. These things didn’t occur to me until much later, after I learned to walk again.
I spent most of the first two years after my stroke getting on with my life. It wasn’t until I was searching for a topic for my thesis that I revisited what happened to me. I had no idea that birth control pills could be so dangerous and I certainly didn’t know that I could have an inherited genetic condition which would make them exponentially more dangerous for me. “How many women have the same condition?” I wondered. “Why don’t we test them before they are put on hormones?” These are some of the questions I sought to answer with my research.
What is Factor V Leiden?
Factor V Leiden (FVL) is a 20,000-year-old mutation common in the general population and a major genetic risk factor for thrombosis. It’s the most common genetic clotting disorder, accounting for around half of all cases. It’s most commonly found in Caucasians (3-8%).
Patients with Factor V Leiden can be either:
- Heterozygous: inherited one mutated gene from a parent
or
- Homozygous: inherited two mutated genes, one from each parent
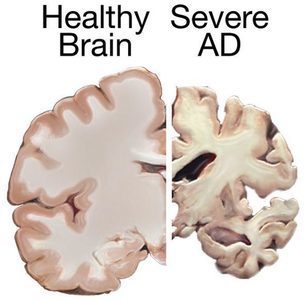
What Does It Do?
As my hematologist described, FVL doesn’t cause blood clots but once activated, it dangerously accelerates clotting. Researchers aren’t clear on why some people with FVL activate and others don’t but there is almost always a precipitating factor—surgery, trauma, immobility, use of hormones, etc.
According to a review in Blood, the journal for the American Society of Hematology, women with heterozygous FVL who also use oral contraceptives have an estimated 30 to 50-fold increased risk of blood clots, while women with homozygous FVL have a several hundred-fold increased risk.
It is the most common genetic cause of primary and recurrent venous thromboembolism in women.
We know that taking estrogen can increase the risk of blood clots, stroke, and heart attack in women. And estrogen, when taken by someone with FVL, can significantly increase the risk of blood clots. Whether women are taking synthetic estrogen in the form of oral contraceptives, or hormone replacement therapy or have increased concentrations of the endogenous estrogens due to pregnancy, they are at much greater risk of clotting.
FVL accounts for 20-50% of the venous thromboembolisms (VTE) that are pregnancy related. In the United States, VTE is the leading cause of maternal death. In addition to causing VTE in pregnant women, FVL has been linked to miscarriage and preeclampsia.
Perhaps the women most at risk for blood clots are those that have been placed on hormone replacement therapy (HRT). A recent review of data from several studies found that women taking hormone replacement therapy were at an increased risk of blood clot and stroke. Worse yet, women with FVL who are also on HRT were 14-16 times more likely to have a VTE.
Despite these risks, women are not systematically tested for FVL before they are prescribed oral contraceptives, before or during pregnancy, or before commencing HRT.
What Women Know about Birth Control and Blood Clots
Part of my thesis research included a survey to assess what women understand about the risks of birth control pills and clotting disorders. Over 300 women who had taken birth control pills participated. What I found was that most women do not understand the side effects of hormonal birth control, nor are they familiar with the symptoms of a blood clot.
As for clotting disorders, nearly 60% of the women surveyed had no knowledge of these conditions. When asked whether they knew about clotting disorders BEFORE they took birth control pills that number increases considerably.
Over 80% of women were taking a medication without the knowledge that they could have an undiagnosed genetic condition that would make that medication exponentially more dangerous.
This shouldn’t come as much of a surprise give that this information is not found in advertisements for birth control pills, on non- profit websites about birth control pills and their risks, or on literature provided with the prescriptions.
Why Aren’t Women Tested for Clotting Disorders?
The most common reason I found in my research for not testing women were cost-benefit analyses measured in cost per prevention of one death.
Setting aside the moral argument that you cannot put a price on a human life, because clearly the government and corporations do just that. (It’s $8 million in case you were wondering.) The cost of taking care of taking care of victims of blood clots is not insignificant.
Each year thousands of women using hormonal contraceptives will develop blood clots. The average cost of a patient with pulmonary embolism (PE) is nearly $9,000 (for a three-day stay not including follow-up medication and subsequent testing).
A hospital stay as a stroke patient is over twice that at nearly $22,000 (not including continuing out-patient rehabilitation, medications, testing, etc.). As a stroke survivor, I can tell you that the bills don’t stop after you leave the hospital. I was incredibly lucky that I only needed a month of out-patient therapy. Most patients need considerably more and will require life-long medication and testing. It’s important to note that due to the increasing cost of healthcare, the figures in these studies (PEs from 2003-2010; strokes from 2006-2008) would be exponentially higher now.
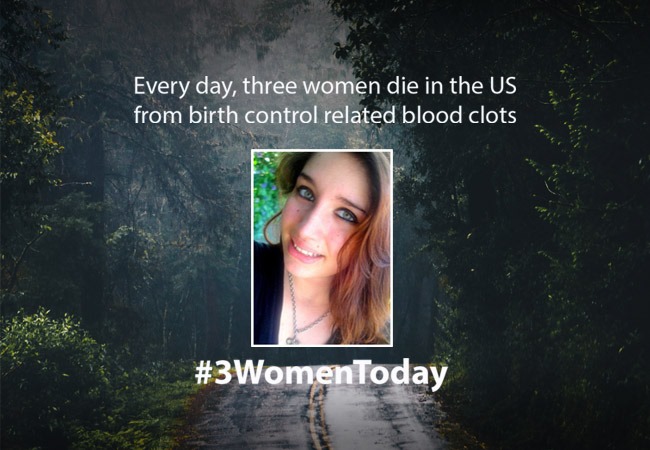
I’m not a statistician but I can do some basic math and while I wasn’t able to find data for the United States (surprise, surprise), the health ministry in France recently conducted a study that showed that the birth control pill causes 2,500 blood clots a year and 20 deaths. The United States has 9.72 million women using the pill compared to France’s 4.27 million. This doesn’t include the patch, ring, injectable, or hormonal IUD, but for the sake of keeping things simple, let’s just use the pill. So we have over twice the pill-users as France, which means twice the blood clots (5,000) and twice the deaths (40). If we assume that half of the blood clots are PE and half are stroke, we come up with a whopping $77.5 million in hospital bills for these blood clots (not counting life-long treatment). Now adding the cost-of-life determined by the government (40 women times $8 million= $320 million) and we end up with nearly $400 million a year in damages caused by the pill. For the cost of only one year of damages, all 10 million women could have a one-time $40 blood test which would result in considerably fewer blood clots.
Furthermore, the research in my thesis shows that women would be willing to not only take these tests, but also to pay for them!
Of the 311 who answered the question, 82.3% (or 256) said they would be willing to take the test. Only 7.2% said no, with the other 10.6% “not sure.” More than 60% of respondents would be willing to pay for the test (up to $50).
In addition, the cost of a blood test is directly proportional to how frequently it is performed. An increase in testing will result in a decrease in the cost of testing.
Women Deserve Better
Putting aside the monetary costs for a moment, what about the emotional and physical toll for women who suffer these dangerous and debilitating blood clots? There is no excuse for women to suffer strokes, pulmonary embolisms, DVTs, multiple miscarriages, and still births because they have an undiagnosed clotting disorder.
That said, requiring a test before prescribing hormones to women would raise awareness of the dangers of these drugs and may reduce the overall number of women using them. Which leads one to wonder if the absence of testing for women is really just a public relations strategy.
Perhaps one of the most devastating cautionary tales of not testing for clotting disorders comes from Laura Femia Buccellato. Her daughter Theresa was 16 years old when she was killed from a blood clot caused by (undiagnosed) Factor V Leiden and birth control pills. Would Theresa be with us today if she had had a simple blood test? Would I have had a stroke? When we will demand better?
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by fernando zhiminaicela from Pixabay.
This article was first published in September 2016.