As a health journalist and a co-founder of Endo Warriors, a support organization for women with endometriosis, I often get asked “what is endometriosis?”
Which is funny since it is estimated that 176 million women worldwide have endometriosis and yet no one knows about this global health issue.
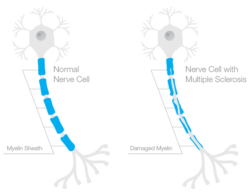
Sometimes I say “it’s a secondary autoimmune disease where the lining of the uterus is found outside of the uterus and throughout the abdominal cavity — to varying degrees — causing chronic pain and infertility.
And other times I say “it sucks.”
Nancy Peterson of the ERC said “If 7 million men suffered unbearable pain with sex and exercise and were offered pregnancy, castration or hormones as treatment, Endo would be a national emergency to which we would transfer the defense budget to find a cure.” And, I don’t disagree.
If 7 million American men had unbearable pain every time they ejaculated, no one would ever suggest chopping off their balls. If they went to a health clinic that also offered pregnancy prevention services, we wouldn’t shut those clinics down. If 7 million American men were in pain every time they masturbated, urinated or tried to have sex we wouldn’t tell them “it’s all in their head” or “to take the pain like a man.” No, we would listen and try to find them a cure that didn’t include castration or drug-induced de-masculinization.
But that’s not the case.
Instead we have 7 million American women with chronic pain related to the tissue in their uterus and their menstrual cycle. 7 million American women who have pain before, during and after their menstrual cycle. 7 million American women who experience pain while exercising, having sex and going to the bathroom. So we offer them chemical-menopause and hysterectomies and when those don’t work we throw our hands up in the air and say “well, at least I tried.” Better luck in your next life, perhaps you’ll come back as a man.
The menstrual cycle is the butt of all jokes directed towards women. Bad day? Is it your period? Is Auntie Flo in town?
Seeing red? Are you on the rag?
No, actually I’m just mad that the idea of healthcare for women makes people want to cover their ears and run screaming.
Free birth control for women?
Great idea!
That is until some political pundit insinuates women should just learn to shut their legs.
Maybe instead we should learn to listen to the myriad of women on birth control for issues beyond planning pregnancies. Maybe women should just get easy access to low cost birth-control without having to recite their medical record.
October is health literacy month and when it comes to health literacy, Americans are kindergartners trying to eat the paste off their fingers.
We think Obamacare and the Affordable Care Act are two different things; getting outraged at the notion of Obamacare yet think the idea of ‘affordable’ healthcare is quite nice.
Access to low-cost health care for everyone? Let’s shutdown the government!
Rather, if we want the government out of our private healthcare, then how about they get out of our uteri as well?