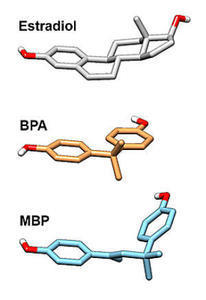
An oft repeated theme in this journal is that measurement matters. From the basic concept that one cannot manage what is not measured to the more specific notion that research protocols in the lab should attempt to mimic real life as much as reasonably possible, we believe measurement is critical. In matters of health and hormones where complex systems with a myriad of ever-changing variables are the norm, this is difficult at best. Sometimes, however, the simple act of measuring these variables opens a world of insight. This is the case with BPA and other estrogenic plastics.
BPA and Estrogens
Bisphenol-A (BPA), the estrogenic activator leaching sperm from our men and damaging the ovaries of women came to the world’s attention several years ago after a vocal and strident outcry from moms. The FDA subsequently remitted, prohibiting BPA from baby bottles and sippy cups and a slew of newer ‘safer’ BPA-Free plastic products emerged, but are they really safer? Maybe not.
Simulating Real Life Usage: Measurement Matters
Until recently, no one had measured the estrogenic activity of the other compounds used to plasticize our food containers. Nor had anyone measured these compounds under real-world stressors, such as UV-radiation (sunlight), microwave radiation or in the dishwasher or with different types of solvent (to represent the food/drinks contained by these plastics). Indeed, as is often the case, we were lulled into a false sense of safety. We believed that since BPA was removed from plastics, the endocrine disruptors were also removed, when in fact the other compounds had simply not been measured.
As one might expect, once those tests were conducted, researchers found that most plastic products on the market today release chemicals that are estrogenic – even those marketed as BPA-Free. Baby bottles, where much of the BPA outcry began, can leech as many as 100 different chemicals especially when exposed to real-life stressors, sunlight, microwaves and dishwashers, all estrogenic in nature.
Sunlight, in particular, was especially adept at maximizing the release of estrogenic chemicals into the solvent. Who hasn’t left their water bottle in the car? And when the plastics were tested in both polar and non-polar solvents (most foodstuffs/drinks are a combination of both), the majority showed reliably detectable estrogenic activity.
What to Do With All of These Estrogens
Not to worry, according to the authors of the study, there are ways to create plastics that don’t elicit estrogenic activity and they don’t cost any more or require different manufacturing than those that do. It’s simply matter of choosing to utilize those plasticizers and associated chemicals instead of what we currently use. The question is whether major plastics manufacturers will pay heed to these warnings and make the switch. Did I mention the man-boobs and infertility from the extra estrogens?
The study: Most Plastic Products Release Estrogenic Chemicals: A Potential Health Problem That Can Be Solved
Postscript
The article above was published originally in October 2012. Over two years later, I am sad to say that not much has changed. Industry has repeatedly denied the safety issues with BPA and the other, presumably safe, BPA-free plastics. The current campaigns, much like those of the tobacco industry, proffer industry financed research as proof of product safety while discrediting any scientist who brings evidence to the contrary. It’s a common script followed by all chemical manufacturers; one that has yet to be successfully curtailed.