I don’t particularly like saying I’ve been “victimized” nor do I like thinking of myself as a “victim”. I never have. The truth is though, according to the Merriam Webster Dictionary, I have been victimized. Merriam defines victimized as follows: to treat (someone) cruelly or unfairly: to make a victim of; to subject to deception or fraud. Victim is defined as: a person who has been attacked, injured, robbed, or killed by someone else; a person who is cheated or fooled by someone else and someone or something that is harmed by an unpleasant event (such as an illness or accident).
In 2007, I was knocked out with Versed and surgically assaulted. I wrote about what happened to me here. The reason I use the word “assaulted” is because I did not consent to surgery – more specifically I did not consent to castration. Indeed, I was treated cruelly. I was attacked, injured, and robbed.
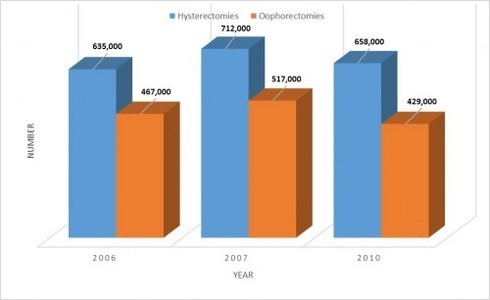
When there is no consent for surgery, it’s absolutely considered assault and battery. With over half a million women undergoing hysterectomy each year, it’s hard to imagine that there is informed consent in all of those cases – really hard to imagine. It would be bad enough if women were only up against hysterectomy and castration abuse, but sadly, there are many more ways women are being abused and victimized by medicine. You can read more about that here.
So what’s a victim to do? How does a victim start over and find purpose in her life again? Where exactly does a victim turn for help? How does a victim heal from the trauma? I suspect the answers to these questions might differ from one victim to another. The answers would also likely depend largely on the circumstances. And, while I can’t answer for other victims, I can certainly explain how I’ve managed to go on and even find purpose again.
One of the most important steps I took was to reach out. I know from experience that it is never a good idea to isolate oneself – although it is often human nature to do just that during times of trauma. For me personally, I knew that I needed to contact lawyers to see how I might go about pursuing a medical malpractice suit, since I did not consent to surgery.
I also contacted the police to see if filing criminal charges was an option for me. I found out it wasn’t because, according to the police officers I spoke with, it’s considered a “civil” case when a person’s been harmed by a doctor inside a hospital. More regarding how I feel about that another day though.
I reached out to local lawmakers and testified in both Indiana and Kentucky regarding hysterectomy informed consent laws or rather the lack of them. And last but not least, I reached out to other women who’ve been abused by medicine. Sadly, there are many – too many.
And while contacting lawyers, police, lawmakers, and other women made make me feel less like a victim externally, I still felt like a victim internally. I have never allowed myself to assume the role of victim and I didn’t want to do that in this case either. I searched my heart and knew what I needed to do. I needed to write. So, I created a blog site here and then a website here and eventually a Facebook page here. And, I’ve written a variety of articles for Hormones Matter as well.
The way I process, heal and communicate is through my written words. Ultimately, as negative and painful as undergoing unconsented hysterectomy and castration has been for me, it forced me to connect with and understand who I am at the deepest level of my being. When my former doctor took the violent actions he did against me, something so precious –so incalculable- was taken from me in that instant: my value and my worth – as a human being and especially as a woman. I had to dig deep to find myself again. I’m still digging…
As the anniversary of my surgical assault draws near on September 27, I can’t help but think about that day that changed my life, health and sexuality forever. I’ve asked myself over and over again why was I targeted for unnecessary surgery and why was I knocked out against my will, sliced open, and castrated. This is what I have concluded. During the two hours I was in surgery, I was nothing more than an object that happened to possess the pieces or body parts necessary to make money for that doctor and that hospital. Behind those surgical doors, I was treated as property (though never purchased), that my former doctor felt he had the right to touch and use for his own purposes.
During those two hours, I had no voice, no thoughts, no feelings, no soul, no mind, no emotions, no power and no potential. I only had a vagina and the life-sustaining organs that lived inside of it. And he felt entitled to that – entitled to take away my life-sustaining organs and my womanhood without actually knowing or caring anything about me. He violated me in the worst possible way one human being can violate another human being. That doctor ruined my life, my sexuality, and my health without even the slightest regard for how profoundly my life would change. Every dream I carried inside of me was crushed beyond recognition because of what he did with his scalpel.
If there’s one thing I’ve learned through this nightmare experience, it’s that I have to speak out about what happened and call things the way they are – even if that’s not necessarily what others are comfortable hearing and knowing.
I don’t sugarcoat what happened to me. I can’t. What was done to me was violent, shameful, wrong, immoral, unacceptable and downright evil. It was painful, hurtful, disrespectful, discriminatory, barbaric and criminal. I try to soften the trauma of what happened by reaching out to other women who’ve been victimized to let them know they are not alone in their devastation.
And, of course, my hope is to help women who’ve not yet been victimized know the truth about hysterectomy and castration that their doctors simply will not tell them. In other words, in helping other women, I’m taking the horror of what happened to me and I’m turning it into something of worth. I’m turning my pain into something I can at least live with and not lose my sanity completely.
I feel. I connect. I cry. I learn. I speak. I fight. I write.
The devastation I’ve endured in this situation is matchless to anything I have ever experienced before other than the loss of my two youngest children. There’s no way I can say it isn’t. At my weakest moments, I remember my strength. I remember that I have a voice. I speak and I speak loudly. I speak not only for my own sake, but for the sake of millions of other women. When I tell my story, I’m telling the story of all women who’ve been abused and victimized by medicine. Knowing I am helping someone else, helps me survive.
Speak Up! Speak Out!
I would love for more women to take a stand with me against the medical abuse of women. Please consider sharing your own story on the Hormones Matter site. Let’s connect and see what we can do together as one large voice!
We need your help.
Hormones Matter needs funding now. Our research funding was cut recently and because of our commitment to independent health research and journalism unbiased by commercial interests, we allow minimal advertising on the site. That means all funding must come from you, our readers. Don’t let Hormones Matter die.
Yes, I’d like to support Hormones Matter.
This post was published originally on Hormones Matter in September 2014.