It appears that high doses of vitamins B1, B6 and B12, administered separately or in combination, can alleviate acute pain by potentiating the analgesic effect of non-opioid analgesics such as diclofenac (an NSAID), sold under various trade names. These facts were published in a German paper. In addition, a randomized, double-blind, controlled clinical study was reported in 378 patients with lumbago. The term lumbago is a relatively old one and it is now often referred to as “back strain”.
The patients were divided into two groups, half of them receiving diclofenac together with very large doses of vitamins B1, B6 and B12. The other half received only diclofenac . The investigators concluded that the addition of the B vitamins did indeed enhance the analgesic effect of the drug. The primary mechanism for the anti-inflammatory, anti-pyretic and analgesic action of diclofenac is thought to be by a biochemical mechanism that is well known in the body and described in the paper.
When I read this, I became aware that the mechanism they were describing was the same mechanism that has been described for one of the actions of thiamine tetrahydrofurfuryl disulfide (TTFD, Allithiamine, Lipothiamine) a thiamine derivative that I have mentioned a number of times in posts on this website. When I further researched the mechanisms of action of diclofenac, I read that “diclofenac also appears to exhibit bacteriostatic activity by inhibiting bacterial DNA synthesis”. Could it be that the drug has an effect on mitochondrial DNA in people using it to relieve their pain? If so, this would be a serious indictment on its use.
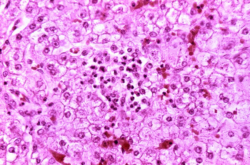
Mitochondrial DNA
We now have reason to believe that our mitochondria (cellular energy producing organelles) have evolved from an original bacterium millions of years ago, and we now know that they have their own genes. These genes, inherited only from the mother, are completely separate from the cellular genes that we inherit from both parents. They are vitally important in the function of mitochondria that are responsible for synthesizing ATP, the energy currency used by the body. The interesting thing is that mitochondrial DNA is like bacterial DNA, has a different conformation from that of cellular DNA, and could be expected to be sensitive to the “DNA related bacteriostatic activity” reported to be one of the effects of diclofenac.
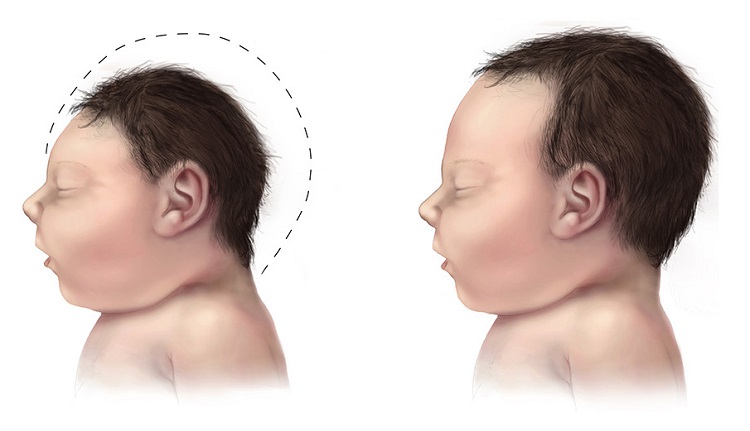
Side Effects of Diclofenac
There are 50 side effects of diclofenac recorded online. It may surprise you to know that 20 of the symptoms reported as side effects are identical to those that are well known in relationship to the thiamine (vitamin B1) deficiency disease, beriberi. Since thiamine is vital to the normal function of mitochondria, perhaps it suggests why three members of the vitamin B complex enhance the analgesic effect of the drug by protecting the patient from harm. This would enable it to be used with reduced dose, thus obviating the possible appearance of side effects.
Side Effects of Pharmaceuticals
It is always wise for a patient who is taking a drug to know what the potential side effects are. With this story of diclofenac, I was reminded of a drug that was produced in the 1930s in order to stimulate weight reduction. The chemical name is dinitrophenol (DNP). The side effects were so severe and occasionally caused sudden death, so it was withdrawn in 1938. Its present use is in experimental research in animals because it inhibits mitochondrial function and enables the researcher to study energy metabolism. Believe it or not, DNP is still available for weight reduction. There is no doubt that it works but it certainly offends the Hippocratic oath accepted by all physicians, “thou shalt do no harm”.
Genetic Susceptibility
We simply do not know the genetically determined susceptibility of an individual in the use of a foreign agent prescribed to relieve a given symptom. The body always recognizes a “foreigner” and sets about breaking it down and getting it out of the body as quickly as possible. If a vitamin is used in a much larger dose than merely replacing it as an essential nutrient, it may be thought of as a drug. This is really a new concept in medicine and has not yet reached the collective psyche of medical practice. Perhaps the body recognizes the huge dose, but uses what it needs and excretes the excess. The trouble with that is that the present concept is that vitamin replacement is thought to be confined to the tiny doses found in natural food that are required by a healthy individual. No thought has been given to the fact that a vitamin may have to be used in order to stimulate and restore the decayed effectiveness of the enzyme to which it must bind. It is as though the roles of the enzyme and the vitamin are reversed. In a sense, the enzyme becomes cofactor to its requisite vitamin rather than the normal enzyme/cofactor relationship.
Energy Metabolism is the Core Issue
What seems to be emerging from all this is that failure of energy metabolism, coupled with genetic risk and the imposition of individual life stresses, provides us with a new medical model for disease. Besides killing the “enemy”, the bacteria, viruses or cancer cells safely, the only real treatment possible is an educated use of nutritional components to coerce damaged cellular systems back into a state of functional efficiency. Healing takes energy and only the body knows how to do that. We should give it every possible assistance. There is much evidence that even cancer cells become maverick because of devious energy metabolism.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by Inge Poelman on Unsplash.