In 2011, I published a paper that pointed out the large overlap between estrogen-sensitive cognitive functions and cognitive features that are commonly impacted in autism (1)(2)(3). These overlapping factors include anxiety (4), motor deficits (5), stereotyped and repetitive movements (6), epilepsy (7), hyperactivity and attention deficit (8), disrupted pain recognition (9), deranged serotonin system (10), atypical memory function pattern (11), and atypical visual-spatial information processing (12). From this data and what is known about animal physiology, I developed a theory that excessive estrogen-sensitive brain growth during gestation could cause a high-functioning form of autism.
The brains of lower mammals are most receptive to estrogen-sensitive growth during the gestational period of sexual differentiation, when the fetus’s testosterone enters the developing brain, converts to estradiol, which is an estrogen, and proceeds to stimulate estrogen receptors. Counter-intuitively, it is this estrogen-sensitive development that makes the male brain masculine (13). The human brain is sexually dimorphic in the same areas known to be rich with hormone receptors in animals, suggesting that human development may proceed similarly (14).
If some estrogen-sensitive brain growth is necessary for a human brain to become masculine, then there should be a point where this growth becomes excessive and atypical. Male fetuses would logically be more susceptible than females to this excessive growth, due to their relatively higher baseline level of estrogen-sensitive brain development. And if neurodevelopmental autism results after a specific threshold of estrogen-sensitive brain growth is achieved, it would stand to reason that males would be at greater risk than females for developing this form of autism.
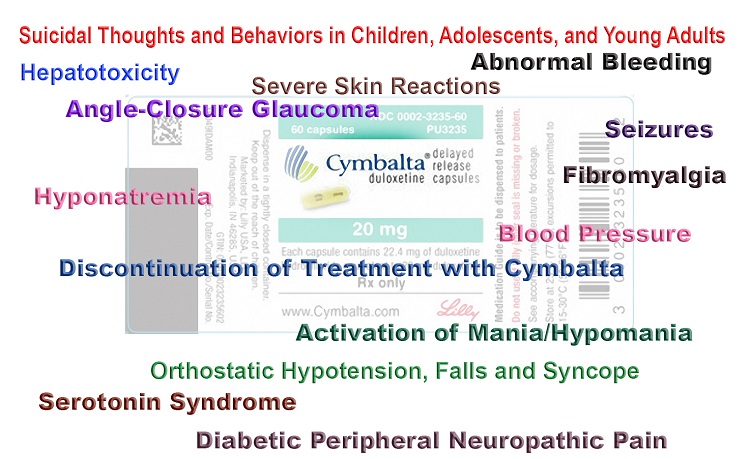
Quite a few studies support a role for estrogen in autism, albeit inadvertently. Hypothyroidism, for example, has been associated with breast cancer as well as increased risk of having an autistic child (15)(16). Autism is also associated with high levels of fetal testosterone, which is relevant because high levels of testosterone would be expected to lead to increased estradiol synthesis (17). One study found a link between autism and mothers’ residential proximity to agricultural application of pyrethroid insecticides during pregnancy, and pyrethroid insecticides are known to be estrogenic (18)(19). Another study found a link between autism and maternal usage of selective serotonin reuptake inhibitors (SSRIs), a type of antidepressant that has also been found to be estrogenic (20)(21). Still another study found a link between autism and maternal vitamin D deficiency, a condition also associated with increased risk of breast cancer (22)(23).
Despite all of the evidence of a link between estrogen and autism development, clearly not all pregnant women who are exposed to pyrethroid insecticides, take SSRIs, or have vitamin D deficiency give birth to autistic children. Why would only some pregnancies be susceptible to excessive estrogen-sensitive brain growth? The answer to this may lie with common genetic impairments that affect the metabolism of folic acid, which has been known since the 1940’s to increase estrogen-sensitive tissue growth in mammals being treated with synthetic estrogen (24).
The Trouble with One-Size-Fits-All Prenatal Vitamins
Folic acid, the synthetic form of the B-vitamin folate, has gradually become a ubiquitous prenatal supplement ever since it was discovered in 1980 to prevent the occurrence of neural tube defects (NTDs). Even though folic acid only prevents NTDs when taken prior to neural tube closure, which occurs four weeks after conception, obstetricians in the United States now inexplicably recommend folic acid throughout the entire nine months of pregnancy (correspondence with author of 25). This may be unwise, because genetic mutations that impact folate metabolism are both exceedingly common and rarely discovered. Such mutations would cause difficulty in metabolizing the large amount of folic acid in most prenatal vitamins.
Folate metabolism is a key part of a critical metabolic process, the methylation cycle, which produces methyl groups that are necessary for numerous biochemical reactions in the body. Vitamin B12 is also required in the methylation cycle. In most commercially available vitamins, unfortunately, B12 is in the form of cyanocobalamin, which requires a methyl group to participate in the methylation cycle. Cyanocobalamin’s demand for methyl groups would therefore place further strain on a genetically impaired methylation cycle that is already struggling to metabolize folic acid, perhaps leading to an accumulation of abnormal amounts of both folate and B12 in the bloodstream. Does a condition of accumulated folate and B12 actually exist in pregnancy? It does indeed – and last year it was associated with an extremely high risk of autism.
In May 2016, Johns Hopkins released the results of a study that measured the levels of folate and B12 in women’s bloodstreams shortly after giving birth. The study involved almost 1,400 mother-child pairs from births occurring between 1998 and 2013. The researchers found that women with very high (more than four times adequate) levels of folate in their blood had twice the risk of having an autistic child, women with very high levels of B12 had triple the risk of having an autistic child, and women with very high levels of both folate and B12 had 17.6 times the risk of having an autistic child (26). Several science journalists and medical news commentators quickly downplayed these findings as being premature, without consideration of possible flaws in current supplementation practice.
The mothers in the Johns Hopkins study were tested for mutations in MTHFR, the gene that provides instructions for making an enzyme critical to folate metabolism. Autism risk did not change based on maternal MTHFR genotype. The participants’ offspring were evidently not genotyped, however, so it may still be reasonable to speculate that the significant vitamin retention discovered by the researchers might have been due to either (a) MTHFR mutations being present in the fetuses, or (b) some combined effect of maternal and fetal mutations. In addition, there are a number of common methylation cycle mutations besides variations in the MTHFR gene that could impact overall metabolic efficiency. In any event, the participants were drawn from a low income population, which suggests that these women may have only had access to relatively inexpensive vitamins containing folic acid and cyanocobalamin. In sum, we have reasonable grounds to suspect that a combination of standard prenatal vitamins and unknown methylation mutations may be the reason why some women would accumulate excessive levels of folate and B12 in their bloodstreams during pregnancy.
Folic Acid’s Forgotten Relationship to Estrogen-Sensitive Growth
One reason that high concentrations of folic acid in a pregnant woman might be problematic is that there is evidence of folic acid acting like a growth magnifier for estrogen. In a series of experiments beginning in the early 1940’s, it was discovered that estrogen-sensitive oviduct growth in chicks was significantly enhanced when folic acid was present in conjunction with the synthetic estrogen stilbestrol (24). Excessive folic acid in the human bloodstream might therefore magnify the effects of estrogenic chemicals in our modern environment – like SSRIs – or magnify the effects of physical conditions that appear to increase estrogen-sensitive growth on their own, like vitamin D deficiency. And perhaps such magnification can cause an excessive amount of estrogen-sensitive growth in a developing human brain just as readily as it does with a growing chick oviduct.
If excessive estrogen-sensitive brain growth does cause neurodevelopmental autism, then the severity of this kind of autism would likely depend on a complex interplay between mother and child’s genetic capacity to metabolize folic acid, the kinds and quantities of vitamins taken during pregnancy, the sex of the fetus, the extent of maternal exposure to factors that promote estrogen-sensitive growth, and the gestational periods in which these exposures occur. A very wide range of outcomes would thus be expected, even amongst genetically similar children.
Superimposed against the variation in autism outcomes would be a potentially wide variation in methylation impairment of the fetus, leading to a highly heterogeneous group of children with varying degrees of neurodevelopmental autism as well as varying degrees of methylation impairment. This assertion is supported by the consistent finding of methylation-related mutations amongst autistic children (27). Adding to the complexity of clinical presentation, some children might develop neurodevelopmental autism without any methylation mutations at all, whereas other children with methylation mutations might escape development of autism because the requisite conditions were simply not present in the womb when estrogen-sensitive brain growth was occurring.
The methylation cycle produces glutathione, and an impaired methylation cycle would lead to lowered glutathione levels and oxidative stress. This, in turn, would cause difficulty in fighting infections, resolving inflammation, and removing toxins like metals from the bloodstream. All of these conditions have been reported in autistic children, in addition to atypical concentrations of glutathione metabolites (28)(29)(30)(31)(32)(33). Vaccines contain metals, and there exists a growing association between methylation impairment and possible predisposition to vaccine injury (34)(35). The estrogen theory would therefore predict autistic children to have more adverse vaccine reactions and related medical co-morbidities than would be predicted to occur by chance alone. The theory would also suggest that post-vaccination regressive autism, occurring suddenly in a child with no prior developmental concerns, may not actually be autism, but may instead be autism-mimicking brain injury (encephalopathy) caused by impaired detoxification pathways failing to purge certain vaccine ingredients. Encephalopathy has, in fact, been repeatedly compensated as a vaccine injury by the federal Vaccine Injury Compensation Program (36).
The Complications of Multiple Avenues of Causation
In closing, it is important to note that the estrogen theory suggests that autism might be a naturally occurring human condition, which has increased in incidence only because (a) widespread folic acid supplementation has magnified the chances of developing it, and (b) the number of estrogenic chemicals in our environment has been, and still is, on an ever-increasing trajectory. It is also important to note that the estrogen theory contemplates genetic susceptibility to autism coming from what might be an entire universe of genetic mutation combinations that compose, affect, or depend upon the methylation cycle, in addition to genes that affect hormone production. Research will never uncover a consistent genetic liability if this is true. In addition, if a multitude of estrogenic substances and conditions are the underlying cause of neurodevelopmental autistic traits, and if vaccines are the underlying cause of regressive encephalopathy and associated medical co-morbidities, then epidemiological studies of prenatal folic acid consumption will likely result in as much uncertainty as genetic studies have.
We Need Your Help
Hormones Matter needs funding now. Our research funding was cut recently and because of our commitment to independent health research and journalism unbiased by commercial interests, we allow minimal advertising on the site. That means all funding must come from you, our readers. Don’t let Hormones Matter die.
Yes, I’d like to support Hormones Matter.
Internet Archive Book Images, No restrictions, via Wikimedia Commons
This article was published originally on Hormones Matter on May 25, 2017.