In the fight against Covid-19, we need all hands on-deck. Whilst vaccination, physical distancing and strong hygiene practices remain priority interventions, one strategy that has received less attention in Western countries is the use of herbal and, in particular, Traditional Chinese Medicine (TCM) as a preventative and potentially therapeutic agent.
Before we dive in, it is important to state upfront that this article in no way seeks to promote TCM as a replacement for vaccination and other critical Covid measures, but rather to understand its potential as a complement to mainstream therapies. Further the application of TCM should always be done under the supervision of a qualified practitioner.
Background on Traditional Chinese Medicine
Traditional Chinese Medicine has been in use for over 2000 years in over 320 epidemics faced by China. Chinese herbal medicine therapy is essentially a mixture of herbs prescribed by Chinese herbalists depending on the patient’s illness and based on core diagnostic patterns (inspection, listening, smelling, inquiry, and palpation). Whilst focus on pathogens is important, treating patients as an organic whole is the focus of TCM hence the central role of herbal compounds which help the immune system and other body systems to prevent and/or respond to pathogens.
The core clinical theories on viral flu-like illnesses were established by Chinese medical practitioners as far back as the Han Dynasty (206 BCE–220 CE) in a foundational text called “The Discussion of Cold-Induced Disorders” (Shang Han Lun) written by Zhang Zhong-Jing. Since then TCM practitioners have continued to learn and evolve their treatments, and today there are over 100 TCMs available for use in treating epidemics.
In modern day China, TCM is routinely used alone and in tandem with Western allopathic medicine to treat a wide range of different health conditions. Similar branches of medicine are used in South Korea, Japan and other parts of Asia.
Traditional Chinese Medicine and Covid-19
Since the beginning of the Covid-19 outbreak in Wuhan in late 2019, TCM was widely deployed across China to slow down the surge in infections. This was in part influenced by the Chinese experience with using TCM during the SARS epidemic. Studies found that when compared with Western Medical Treatment alone, TCM could help to reduce SARS fatality rates, improve oxygen saturation in critically ill patients, and alleviate symptoms such as dyspnea. Other studies by Luo et al. in 2020 and Lau et al in 2005 found that TCM was an effective preventative measure for SARS.
Soon after Covid-19 appeared in China, the National Administration of Traditional Chinese Medicine (NATCM) commissioned a team of experts to develop a traditional Chinese herbal medicine treatment program for the virus. On 24 January 2020, the first case of an early stage Covid patient who was cured by TCM was reported in Beijing.[1] The following day, another cured patient was reported.[2]
On 27 January 2020, an updated traditional Chinese herbal medicine treatment program was issued by China’s National Health Commission and NATCM which required health authorities to use traditional Chinese herbal medicine alongside Western medicine in the treatment of Covid-19.[3] TCM practitioners break Covid down into seven different stages (prevention, observation, initial, middle, severe, critical and recovery), with different herbal treatments prescribed for each.
In March 2020, another clinical case went public showing that a herbal formulation recommended by China’s National Health Commission was effective in attenuating acute respiratory distress syndrome in a mild Covid-19 patient.
Since then several further case-studies and reviews of TCM used during the Covid-19 pandemic have been published demonstrating TCM’s therapeutic effects. One such review, published last November concluded:
The combination of western medicine and TCM in treatment [is] of great significance for the prevention and treatment of COVID-19.
Effects Are Strongest With Early Interventions
Researchers find that TCM is most effective in addressing symptoms when applied early in the progression of Covid-19. In a May 2020 study of 102 early-stage Covid-19 patients treated with TCM, researchers found that “clinical symptom disappearance time was shortened by 2 days, the recovery time of body temperature was shortened by 1.7 days, [and] the average length of stay in hospital was shortened by 2.2 days”. They concluded that the “early intervention [with] TCM is an important way to improve cure rate, shorten the course of disease, delay disease progression and reduce mortality rate.” and that “the reason why TCM works is not only to inhibit the virus, but [it] might block the infection, regulate the immune response, cut off the inflammatory storm, and promote the repair of the body.’”
Further, Li et al.’s, 2020 meta-analysis showed that herbal medicines are effective in halting the progression of Covid-19 from mild to critical, decreasing hospitalization rates, shortening the duration of hospital stays, as well as alleviating COVID-19 associated symptoms like fever, cough, fatigue, and inflammation.
What Might Be the Mechanisms at Work?
Based on recent in silico results, numerous natural compounds from TCM botanicals have been found highly potent in blocking the enzyme function and membrane receptors of coronavirus.
In a meta analysis of the most used botanicals in TCM for Covid-19 published in October 2020, Huang et al. found the nine most common herbal ingredients were: Glycyrrhizae Radix Et Rhizoma (Glycyrrhiza inflata Batalin), Forsythiae Fructus [Forsythia suspensa (Thunb.) Vahl], Lonicerae Japonicae Flos (Lonicera Japonica Thunb.), Scutellariae Radix (Scutellaria baicalensis Georgi), Platycodonis Radix [Platycodon grandiflorum (Jacq.) A. DC.], Menthae Haplocalycis Herba (Mentha canadensis L.), Gardeniae Fructus (Gardenia jasminoides J.Ellis), Gypsum Fibrosum, and Moschus (Moschus anhuiensis).
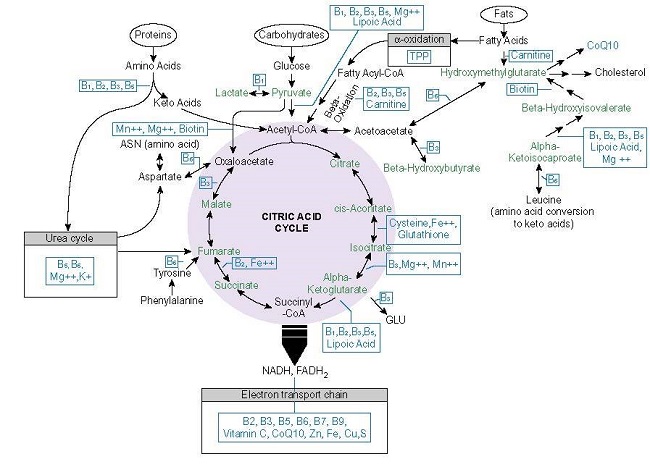
Huang et al’s integrated network analysis on these nine herbs identified eighteen botanical compounds with drug-like potential. Ten of those compounds are flavonoid derivatives. Flavonoids are known to protect cell membranes, and have antioxidant and anti-inflammatory properties.
Huang et al. concluded that the therapeutic effect of these eighteen compounds for Covid-19 was in influencing the COX-2 and MAPK mediated inflammatory pathways. The COX-2 enzyme is induced during inflammation and tissue repair. Data shows that COX-2 plays a role in driving the lung inflammation and injury caused by Covid-19. The p38 MAPK pathway plays a crucial role in the release of pro-inflammatory cytokines such as IL-6 and has been implicated in acute lung injury and myocardial dysfunction. It is thought that the overwhelming inflammatory response in Covid-19 is caused in part by upregulated p38 activity.
Since the compounds studied by Huang et al have been used in dietary supplements for a long time, their toxicity is negligible, which makes them safe to be employed as prophylactic agents, under the supervision of an experienced health practitioner.
In March 2020, Zhang et al screened databases of anti-viral botanical compounds and found 13 compounds that exist in TCM also had potential anti-Covid-19 activity. 125 Chinese herbs were found to contain 2 or more of these 13 compounds, leading the authors to conclude that “Chinese herbal treatments classically used for treating viral respiratory infection might contain direct anti-2019-nCoV [Covid-19] compounds.”
A July 2020 study by Yang et al. went further, examining the active components of two TCMs – Qing-Fei-Pai-Du (QFPD) and Ma-Xin-Shi-Gan (MXSG), both used by the Chinese Government to treat Covid. Their research identified 129 active compounds which fell into four categories: flavonoids, glycosides, carboxylic acids, and saponins. Together these compounds were found to regulate multiple complement, coagulation cascades and thrombin systems to interfere with infection pathways. One major compound in MXSG, glycyrrhizic acid (found in licorice), played an anti-inflammatory role in blocking toll-like-receptors (immune receptors that play an important role in Covid-19) and in suppressing IL-6 production (a predictor of respiratory failure in severe Covid cases).
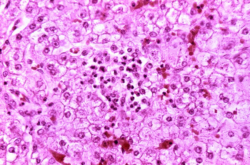
In June 2020, Li et al. published the results of an in-vitro study of the antiviral activity of Lian hua qing wen (LH), a TCM patent medicine comprising 13 herbs, which is a recommended TCM COVID treatment according to Chinese Government Guidelines. They found that the treatment of Vero E6 cells (African Green Monkey kidney cells which have been used for Coronavirus research in cell-culture based infection models since 2003) with LH resulted in an inhibition of SARS-CoV-2 replication and a corresponding reduction in several pro-inflammatory markers at the mRNA level.
A study of Liu Shen, a TCM used widely for treating infectious diseases, which was conducted by Ma et al. in August 2020, found that it exerted inhibitory effects against SARS-CoV-2 replication and virus-induced inflammation in vitro probably via suppressing the NF-κB pathway. This pathway drives the expression of numerous pro-inflammatory genes, including those encoding for cytokines and chemokines. It also plays a role in regulating the inflammasome, which are innate immune system receptors and sensors that activate inflammatory responses in the presence of pathogens.
In a February 2021 paper, Capodice and Chubak highlight several molecules from a wide variety of TCM herbs that have potent antiviral and immune modulating properties in treating Covid-19. Further research is needed to confirm whether these molecules behave similarly when combined together.
What Could All of This Mean?
Whilst further research is needed to dig into the exact mechanisms and full potential of TCM in treating and preventing Covid-19, the initial findings are promising.
Herbal and Chinese Medicine have long been used to treat respiratory illness and viral infections. They have minimal toxicity, can be administered orally and are widely accessible, making them strong candidates for long-term prophylactic use.
Given that those with weaker immune systems are at greater risk of Covid-19 infection, herbal medicines like TCM which can help to modulate the immune system and dampen down the uncontrolled inflammation that occurs in Covid-19, could, as Lei and Liu conclude, offer potential as a preventive or even therapeutic agent alongside other Covid treatments.
As the Covid virus continues to mutate and countries grapple with the tragedy of this Pandemic, all modes of treatment that have minimal risks and proven benefits should be given serious consideration. Herbal and Traditional Chinese Medicine may be one such contender.
Additional Notes
[1] Article reads: “A patient diagnosed with 2019-nCoV pneumonia was discharged from Beijing”
[2] Article reads: “One patient with 2019-nCoV pneumonia was discharged today in Beijing, with a total of two discharged”
[3] Pneumonitis Diagnosis and Treatment Program for New Coronavirus Infection (Trial Version 4). In. Edited by The General Office of the National Health and Health Commission of China, Office of the State Administration of Traditional Chinese Medicine. Beijing; 2020.
[4] For example: Ren et al, Traditional Chinese Medicine for Covid Treatment, Pharmacological Research, May 2020; Zhang et al, The clinical benefits of Chinese patent medicines against COVID-19 based on current evidence, Pharmacological Research, July 2020; Zhao et al, Prevention and treatment of COVID-19 using Traditional Chinese Medicine: A review, Phytomedicine, August 2020; Wu et al, Traditional Chinese Medicine as a complementary therapy in combat with COVID-19—A review of evidence-based research and clinical practice, Journal of Advanced Nursing, November 2020; Zheng et al, Efficacy of Traditional Chinese Medicine on COVID-19: Two Case Reports, Feb 2021.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on June 3, 2021