The text below came up on my Facebook book memories recently. It was from a project I worked on three years ago. I never did anything with this particular bit of insight, and apparently, completely forgot about it. Since it may have some bearing on COVID-related thrombosis, a quick search suggests that possibility (here, here, here), I thought I would publish the text so that others may follow up.
Cardiolipin: A Mitochondrial Response to Stress
I just learned something interesting. Am working on the project regarding testing women for clotting disorders prior to receiving a prescription for hormonal contraceptives, which induces clotting and thus exacerbate thrombosis risk. Antiphospholipid syndrome (APS) is a common contributor to clotting – think Lupus, RA, but many other disorders. One of the antibodies involved in APS is called anti-cardiolipin (aCL).
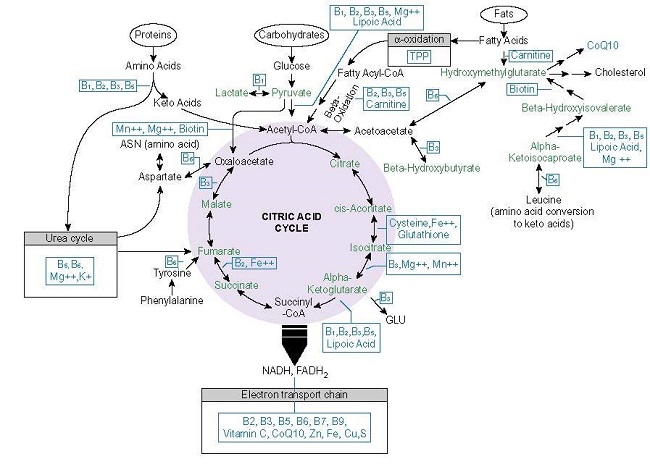
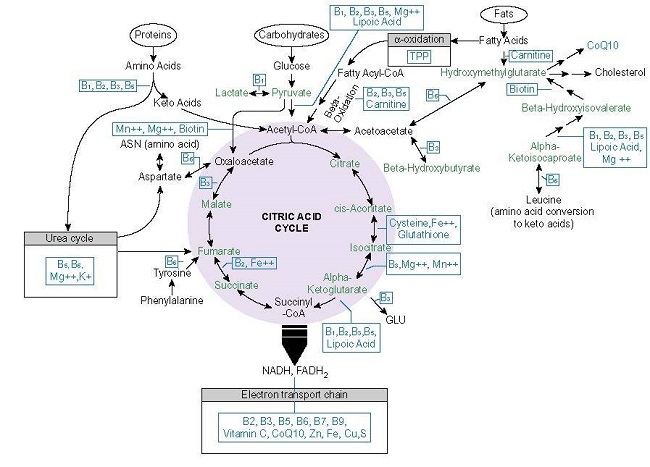
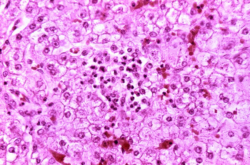
Cardiolipin is a mitochondrial antibody produced in by the inner membrane of the mitochondrion, involved in a bunch of functions, including complex IV of the electron transport chain (ETC), apoptosis, and other stuff. Cardiolipin moves to the outer mitochondrial membrane when the mitochondria are stressed (in response to pharmaceutical toxicants, nutrient deficiencies, etc). Once outside the membrane antibodies form to attack it because it is not supposed to be there, APS develops and all sorts of things go wrong.
First insight: APS is mitochondrial in origin and is a response to environmental cues. This suggests that what we call autoimmunity is mitochondrial in nature as well – inner membrane molecules displaced to the outer membrane and then recognized as threats or toxicants and acted upon accordingly. Second insight, the body is doing what it is supposed to do. It’s dealing with a threat. It is not autoimmunity in the sense of aberrant immune function (something I never bought anyway). The problem is that the threat never resolves. So if we were to resolve the threat – repair the mitochondria and remove the toxicant exposure, the immune response should resolve. The molecule should return to its appropriate home and immune cascades against it settle.
Unrecognized APS Cascades and COVID
Additionally, let me add a bit of background about APS. The text below is from our report, which is available on ResearchGate.
Antiphospholipid syndrome (APS), also called Hughes Syndrome, is an acquired autoimmune condition of unknown origins with hypercoagulability and a high rate of thrombosis. It affects predominantly women, increases with age and comorbid diseases such as systemic lupus erythematosus (SLE), Sjogren syndrome, and rheumatoid arthritis (RA). Up to 70% of SLE patients and 28%of RA patients respectively test positive for antiphospholipid antibodies. It should be noted that 1-5% of the general population also test positive for APS, but remain largely asymptomatic. This is likely attributable to the environmental reactivity of the antibodies. Common medications, including hormonal contraceptives, antibiotics, and vaccines induce APS chemistry. APS shows an elevated risk for both venous (70%) and arterial (30%) thrombosis. It is estimated that 30-40% of patients will develop thrombosis at some point in their lives and 15% of DVTs are attributable to APS. Myocardial infarction and CVTs are common among APS individuals. Of note, a study covered in the ‘cost of not testing’ section, found Lupus antibodies, one of the markers of APS, to be the most commonly identified thrombophilia in their hospital. APS may be among the more common causes of acquired thrombophilia, especially in women.
Diagnosis of APS is difficult, relying heavily on clinical acumen. Laboratory testing requires the measurement of antiphospholipid antibodies (anticardiolipin, lupus anticoagulant, beta 2 glycoprotein – B2GP1) done at repeat intervals 12 weeks apart. The tests are highly reactive to environmental factors, including acute phase thrombosis, infections, and medications. For these reasons, the indicated prevalence rate is likely inaccurate.
Connections to Explore
Given the environmental trigger of APS antibodies, including cardiolipin, and the apparently high but unrecognized prevalence of variables that predispose one towards APS reactions, I cannot help but wonder if a portion of the clotting seen in COVID patients is related to these pathways triggered by either virus itself and/or the medications used to treat the virus. Similarly, given the lack of diagnostic acuity with APS, is it possible that a percentage of the COVID patients have activated but latent APS cascades in advance of developing COVID? Finally, with cardiolipin antibodies identified in COVID patients, does that not tell us that tell us that we ought to be looking more closely at the mitochondria in our treatment protocols?
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.