PCOS and Irregular Periods in Teens
Polycystic Ovarian Syndrome (PCOS) is one of the most common hormonal disorders for women. It is both a metabolic and endocrine disorder, which means it affects insulin production, metabolism, and reproductive hormones. Contrary to its name, it doesn’t necessarily mean you have polycystic ovaries. In fact PCOS has many different faces. PCOS symptoms include irregular periods, difficulty conceiving, hirsutism, acne, and obesity. Research is now uncovering that you may not exhibit any of these symptoms but still have the disorder. This means that PCOS is either commonly misdiagnosed or not diagnosed at all.
The standard treatment for teenagers with irregular periods is hormonal contraception. On the surface it seems to fix the problem. It gives them a regular bleed and often clears up pesky acne. The seemingly regular ‘period’ is deceiving, however. It is not a menstrual cycle. There is no ovulation while on hormonal contraceptives and the bleeding is simply what is called a ‘pill withdrawal’ bleed; meaning if she were not to cease taking the pill every month, she would never bleed.
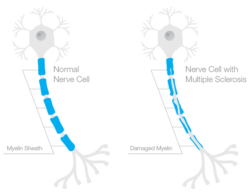
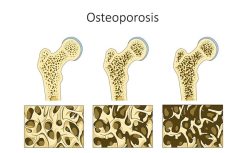
Hormonal contraceptives trick the body into thinking it has already ovulated by providing a steady stream of synthetic hormones, which override brain and ovarian function giving negative feedback to tell the brain to halt any hormone production. In a healthy and functional cycle, there is a wax and wane for all of the reproductive hormones – kind of like an orchestra. All hormones have a part to play. Estradiol and progesterone, the two dominant ovarian hormones, balance each other out and protect bone and heart health as well as the development of the immune system. Having a period is much more than an accessory, it should be considered the fifth vital sign of health for women. A woman on hormonal contraception is not simply not ovulating and menstruating, she is missing out on the benefits of endogenous hormones while also losing time to get to the root issues of her hormonal disorder.
Though it is worth noting that some irregularity is to be expected during the years of puberty, for other girls’ irregularity can be indicative of a hormonal disorder like PCOS. This is concerning since a teenager with PCOS might spend the next 15 years on the pill and not think twice about it. When she is ready to conceive, she will get off of the pill and is likely to find conception difficult, depending on the severity of the underlying PCOS that led to pills in the first place.
Conceiving With PCOS
Since irregular menstruation (and therefore irregular ovulation) is common with PCOS, this is the most obvious obstacle in conceiving. If a woman is not ovulating, she cannot conceive. But that is not the only obstacle in conceiving with PCOS. Women with PCOS often have altered levels of androgens as well FSH and LH which all affect the cycle. Even if a woman with PCOS conceives, if these hormone levels aren’t addressed at the root, a pregnancy could likely need many interventions – as well as the birth and postpartum.
Without proper support, a woman may turn to IVF which might yield a baby, but is unlikely to solve her underlying hormonal disorder. In many cases, IVF could even worsen her health. In this 2014 study researchers concluded:
“Women with PCOS are at an increased risk of adverse pregnancy and perinatal outcomes, which could not be explained by assisted reproductive technology. These women may need increased surveillance during pregnancy and parturition. Future research would benefit from focusing on glucose control, medical treatment and hormonal status among women with PCOS during pregnancy.”
Postpartum and Lactation With PCOS
We know that the more interventions that are needed in a pregnancy and birth, the more the risk of trauma and stress increases. Birth interventions often delay lactogenesis II, the stage of milk production where colostrum transitions to the white viscous milk that we commonly think of when we imagine breastmilk. This transition usually occurs within 24-48 hours after giving birth, but we often see it delayed as long as 4 or even 5 days after a traumatic birth.
Furthermore, while research is still developing in this area, there is enough data to support the idea that PCOS (and its accompanying insulin resistance) plays a major role in milk supply. This study showed that a particular gene is expressed more prominently when a mother is insulin resistant, than in insulin-sensitive individuals. This gene is intricately tied to milk production.
Milk Supply and Insulin Resistance
Let’s talk about breast milk supply for a minute. The two main things that drive milk supply: 1) prolactin production (think baby or pump suckling on nipple, this corresponds with surge in prolactin) and 2) sufficient glandular tissue. As a lactation counselor, when someone comes to me with “low supply”, the first thing I need to parse out is if this issue is baby sourced or parent sourced. Does mom have an adequate supply, but the baby isn’t able to get it and the body responds in classic supply demand fashion by lowering the supply OR is the mom truly unable to make a full milk supply? Clinically it is usually the first option, but occasionally it is the second.
To make an adequate supply on the mom’s side, she must have sufficient glandular tissue. This means that the breast tissue grew appropriately at the time of puberty as well as during pregnancy (this is the final stage of maturation for breast tissue). And of course, it needs to contain enough milk ducts. We know that insulin has a direct action on the mammary glands during breast development. To develop adequately, breast tissue cells must remain insulin sensitive. In this study on mice, “It was found that both IGF-1 and IGF-2 activate the expression of milk protein β-casein in the presence of prolactin and hydrocortisone. It was found that β-casein expression is accompanied by cyclin D1 co-expression.” This means that fewer receptors = fewer milk ducts. And most importantly, this means that breast development during puberty has implications later on in reproductive life.
Moms with Hypoplasia, or Insufficient Glandular Tissue (IGT), don’t all have the same breasts. Size is not indicative of the quantity of glands. IGT breasts can be big, small, medium, round, flat, high or low – the only thing they all have in common is that the glandular tissue is simply not sufficient to make a full milk supply. The biggest indicator of IGT is if a mom’s breasts do not grow during pregnancy. This is usually a huge red flag. However, with the right support, moms with Hypoplasia can still breastfeed. It often looks like adding in supplementation with either donor milk or formula, and sometimes supplemental nursing systems may be used. Some women with PCOS have lactation troubles, but others do not. Women can have insulin resistance without PCOS, but still have lactation trouble. Women can have PCOS and insulin resistance and have no lactation trouble. While less common and much less understood, women can have lactation trouble (in the form of IGT) without PCOS or insulin resistance.
In the case of a mom with insulin resistance, and especially a missed diagnosis of PCOS, they may have no idea what could possibly be causing their low milk supply. Being labeled “IGT” often feels defeating and devastating. If they struggled to conceive, the mom may feel that their body is simply working against them every step of the way on their journey to motherhood. This increases their risk of postpartum mood disorders and it becomes a bit of a domino effect.
The Importance of Diagnosing PCOS (and Other Disorders) Early
So how do we nip this narrative in the bud? It is a simple answer with a not so simple execution. For starters, health care providers need to prioritize regular, functional ovulation for teenagers. Rather than being put on the pill at 15, struggling to conceive at 30, going through IVF, and having difficulty producing milk – this story could be radically changed at its first juncture. This also extends to women in their 20’s and 30’s and even into their early 40’s – a time when cycles should be regular and functional, unless a woman is breastfeeding (in which anovulation is biologically normal). Hormones change throughout reproductive life. A teenager may have PCOS but the symptoms may not become apparent until after their first birth or during a really stressful period in their life. Health care is fluid and should move along with women as they shift and transition through different seasons in life. The importance of getting an annual exam and pap smear are commonly emphasized to women – but little do we emphasize the benefits of getting a hormone panel done periodically to check in. In some cases, a full hormone blood panel isn’t even necessary. You can get enough information from your symptoms and a Fertility Awareness Based Method chart.
Prioritizing Women’s Menstrual Health
If we are prioritizing functional and regular ovulation for women (and therefore balanced hormones), women can mitigate their symptoms and learn to live with PCOS. While there are no hard and fast cures for PCOS currently, there are many ways to manage it. Some of these variables are in a woman’s control (diet and exercise) while others are much more systemic, cultural, and political such as access to nutrient rich food and health care resources. In industrialized nations, cultural priorities do not often support general health and in modern life, we are exposed to more blue light, less sunlight, and we are chronically over-booked causing higher cortisol levels which also affect insulin sensitivity. But this is a conversation best saved for another day.
It should also be noted that a PCOS diagnosis doesn’t necessitate impaired glucose tolerance. Since PCOS operates on a spectrum (which doesn’t even necessarily correspond with symptoms!), there are many variables at play. The most important takeaway here is that insulin resistance does seem to play a role in breast tissue development and teens with PCOS, which is often misdiagnosed, may miss out on crucial breast tissue development.
In any case more information is critically needed. We cannot ignore this too common condition anymore. More knowledge on hormonal disorders and insulin resistance and lactation deserves to be studied. If you find yourself with either a PCOS diagnosis or lactation struggles, it is worth finding the practitioner who is willing to help you dig deeper and get more answers. This process isn’t easy. There are certainly cases that seem unanswerable, but the more we hear about them, the more we can learn about them.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on June 15, 2020.





















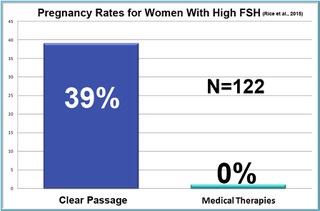 One of the biggest surprises in the ten-year study was in women who were diagnosed hormonally infertile due to high FSH (follicle-stimulating hormone). As a woman approaches menopause, her ovaries demand more and more FSH to stimulate egg growth in older follicles. Measured early in the menstrual cycle, most physicians feel a woman’s FSH levels should be at or below 10 mIU/mL. When a woman’s FSH is above 10, she is considered unlikely to conceive. At FSH of 25, the woman is generally considered to be menopausal.
One of the biggest surprises in the ten-year study was in women who were diagnosed hormonally infertile due to high FSH (follicle-stimulating hormone). As a woman approaches menopause, her ovaries demand more and more FSH to stimulate egg growth in older follicles. Measured early in the menstrual cycle, most physicians feel a woman’s FSH levels should be at or below 10 mIU/mL. When a woman’s FSH is above 10, she is considered unlikely to conceive. At FSH of 25, the woman is generally considered to be menopausal.