I had a recent email from a 38-year-old lawyer to thank me for a treatment that was given to her when she was eight years of age. I do not know what prompted her to try to contact me after 38 years, but her story has to be of general interest because it is so unusual. This eight year old child had a history of crippling asthma and bronchitis for four years. She was so allergic that any kind of mattress exacerbated her symptoms and she was forced to sleep on a plastic lawn chair. When I examined her, her chest was full of the sounds that are typical of advanced chest disease. However, there was a curious observation that turned out to be important. Her body was covered with “goosebumps” and I will try to explain the importance of this later because it made me try an extremely unusual treatment.
I prescribed an oral supplement of 150 mg a day of thiamine hydrochloride. Her symptoms rapidly cleared and all medication was successfully withdrawn. During the next five months she had only two mild attacks of asthma and her weight increased by 6.4 kg (14 pounds). I lost sight of her until the email arrived recently. She told me that over the years she had had only two mild attacks of asthma in her 20s. She had participated in athletic pursuits in college with no problems. The question then is why four years of virtual crippling had been relieved so expeditiously with such a simple treatment. She is now married and has three children all of whom have recurrent episodes of asthma. On further questioning by email, she responded that one of her children develops “goosebumps” if and when she is ill.
More Aspects to the Child’s Medical History
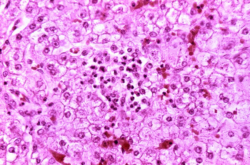
When a patient visits a physician, the reason for the visit described by the patient is called the medical history. An important part of that history requested by the physician is about any illnesses in the family that may be relevant. So in this case the family history revealed that this child’s grandmother had advanced lung and liver disease “of unknown cause”. This suggested to me that the grandmother had an unusual genetically determined condition known as alpha-1 antitrypsin deficiency. This disease originates in the liver because of the genetically determined failure to produce an important substance in the body knows as alpha-1 antitrypsin (A1AT). This is a protein that circulates in the patient’s blood and has an important part to play in preserving the health of the lung. Sometimes, the genetic abnormality in the liver leads to disease in that organ as well as the lung but liver disease does not always occur. However, the absence of the circulating A1AT would inevitably affect the normal function of the lung. It was therefore possible that the eight-year-old child had inherited the lung disease without the liver being affected. Also, this genetic effect can be “silent”, not causing any disease at all, making it possible for this child’s mother to have passed the gene while she herself had no chest disease.
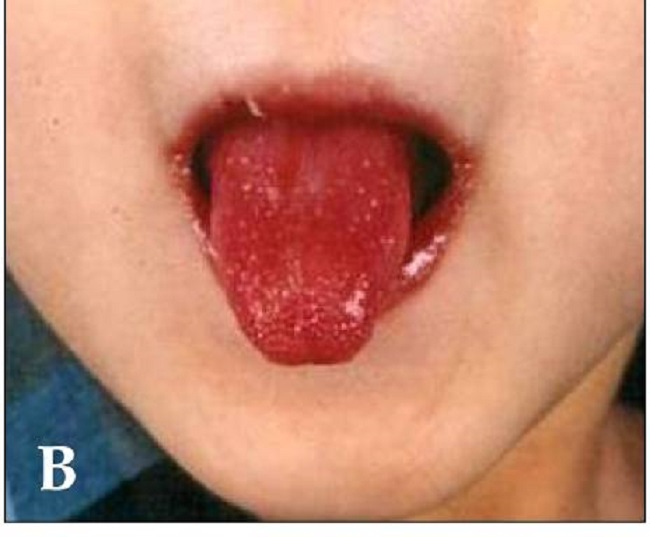
Goosebumps and A1AT Deficiency
The technical name for this phenomenon is piloerection (pilo, a hair). At one time in our evolutionary history the human body was covered with hair like an ape. Some men still have quite a lot of body hair. All these hairs grow out of a tiny organ in the skin known as a follicle. The follicle is also equipped with a tiny muscle that makes the hair stand on end. It is the movement of the follicle by the action of the muscle, whether the follicle contains a hair or not, that creates the effect that we call “goosebumps”. It has been thought that the appearance of our ancestor, with all his body hairs raised, would make him look more aggressive and dangerous, because this action depends on activating the fight-or-flight reflex. Now, I was aware that this reflex is activated by environmental danger. However, thiamine deficiency is perceived by the brain as a source of danger and I concluded that the child’s “goosebumps” might be caused by that. There were other reasons for my suspicion but they involve much more detailed knowledge concerning A1AT deficiency.
The Possible Legacy
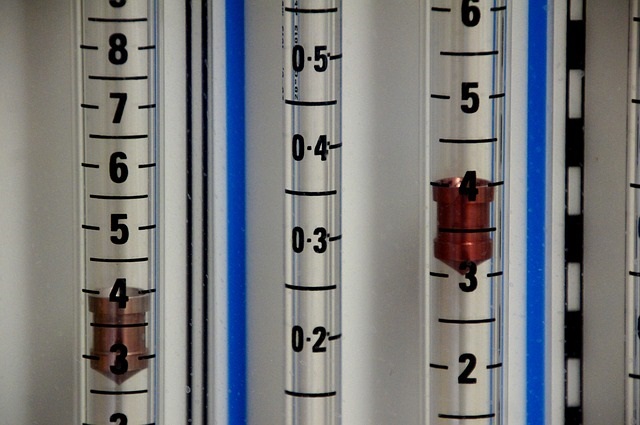
Asthma and asthmatic bronchitis are quite common in children today. Not all of them are as serious as a child that I have just described. However a simple test could be done to ascertain whether A1AT deficiency applies to a given child or even an adult with crippling asthma and bronchitis. The A1AT protein can be measured by a blood test and if it were found to be very low, a trial with megadose thiamine administration could do no harm and might have the dramatic effect that I have described in this child.
This case and many others are detailed in: Thiamine Deficiency Disease, Dysautonomia, and High Calorie Malnutrition.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image credit: https://www.wallpaperflare.com/oxygen-air-medical-mixture-hospital-clinical-care-breathing-wallpaper-wxbmk.