All throughout school I was something of a class clown. The only difference between then and now is that now I have no class. So, it’s no surprise that it was a joke that first made me start thinking critically (some would argue cynically) about the medical industry.
Q: Do you know what they call the person who graduates at the bottom of their medical class?
A: Doctor.
Seriously. This was something of an epiphany for me as a young man. Prior to that, I automatically put all doctors and even the pharmaceutical industry on a pedestal.
I think it serves us well to remember that, for better or worse, doctors are only human. We especially have to keep this in mind in any conversation we have with them regarding birth control. Most of them have been trained to believe in a very rigid dogma that regards The Pill as a panacea.
The Systemic Indoctrination Surrounding Birth Control
Since my book, In the Name of The Pill came out a few months ago, I’ve received several notes from women thanking me because the book gave them information they weren’t getting elsewhere and brought them comfort as they fought against a system that encourages birth control use at every corner. Some have even said the book made them cry tears of joy because it affirmed that they weren’t crazy. It would be impossible to express how meaningful these messages are to me.
I knew before the book came out that the indoctrination of women began at an early age and I knew that it was relentless. From the time they are young girls, doctors browbeat them with conversations about acne, glowing skin, cramps, PMS, fuller breasts, regulating hormones… With all these benefits, one would be crazy not to want birth control. But even being deeply involved, I am constantly reminded that, as a man, I still have no idea just how bad it is.
This weekend, I received an amazing note from a young woman who was only halfway through my book, but she wanted to thank me because she stopped taking The Pill on the one-year anniversary of starting them. She wrote:
“I decided to stop because I came to the realization that for one whole year I hadn’t felt like myself at all. I suffered from extreme paranoia and depression, my hair was falling out in clumps and I felt so fatigued all the time that I couldn’t even see my friends or enjoy my life. I went to the doctor at least once a month with worries and fears about clots and I just couldn’t do it anymore. My body has been struggling a lot coming off of it but mentally and emotionally I am in such a better place and your book has provided me so much comfort in knowing that I’m not crazy!”
You might wonder, “If it was that bad, why did she wait a whole year before she stopped taking them?” But if you’re wondering that, you’re probably a man because most women already know the answer. She continued:
“I tried to go off of birth control once this past year and felt so sick and my doctors persuaded me to go back on it because I ‘obviously need to be using it, if I don’t feel well.’”
Unfortunately, that seems to be a pretty common outlook from the medical field. When you complain about side effects like paranoia, depression, hair loss, or fatigue while you’re on The Pill, they downplay them or dismiss them altogether. But, when you mention feeling bad as your body tries to readjust after you stop the flood of synthetic hormones, that’s proof that you need The Pill.
A little bit wiser the second time around, she took a different approach:
“I have also convinced another close friend to come off of it and we have been supporting each other through the transition – it’s been tough but so worth it to feel like myself…I am now working on healing and am using non-hormonal methods as birth control and feel empowered and liberated!”
The Truth Will Set You Free
I love that she discussed this with a friend and they formed their own support team. It’s no wonder Holly Grigg-Spall, the author of Sweetening The Pill, subtitled her popular book, “How We Got Hooked on Hormonal Birth Control.” As she documents her own struggles to ditch The Pill, she concludes:
“The silencing of honest discussion causes many women to suffer unnecessarily. It wasn’t until I stopped taking the pill that I developed the needed energy, motivation and clarity of thought to express why I had to stop and to question why it had taken me so long to make that decision.”
As simple as it sounds, honest discussion may be the biggest weapon in our arsenal to fight the ubiquitous messages of misinformation coming from the medical community. There is no informed consent. That’s a myth. Our recent citizen’s petition to the FDA demonstrated that even the patient information pamphlets are incomplete. If informed consent is the goal, that information has to come from somewhere. Unfortunately, in the current culture, open and honest discussions among friends are about the only chance a woman has to be informed about the real risks of taking hormonal contraceptives.
Turn the Spotlight on Hormonal Birth Control
Without these discussions (which shouldn’t be limited to women), the damage being caused by The Pill goes unrecognized and leads to under-reporting. It’s hard to believe, but despite the vast number of documented cases of women being harmed by birth control, those numbers are most certainly insufficient in reflecting the real damage being done because people never consider the link.
Let me give you an example. Earlier this year I joined a client on a project that was going to last a couple of weeks. Knowing I was in the final stages of working on my book, he said that he wanted to hear all about it while we were together. He added, “I’m not sure I agree with your position, but I’m willing to keep an open mind. My ex-wife took The Pill for 20 years and never had any problems.”
I told him that it wasn’t my contention that every single woman who took birth control suffered devastating consequences, but that I did think that fact put her in the minority. Over the next two weeks, we had several in-depth conversations about The Pill, my research, the political landscape, and the broad range of side effects.
In the end, I’m still not sure he was completely convinced, but he did offer this, “I have to tell you, my ex-wife had breast cancer and had her gallbladder removed but we never even knew it could have been related to The Pill.”
The more we all discuss these things – the more the damage will be brought out into the light. That’s why one of the shortest reviews of my book on Amazon may be my favorite. A reader named Melissa wrote:
“Very educational makes me want to start a study group and have each member do a study on 3 family members that have taken the pill to see results.”
Wow, that sends chills down my spine. Can you imagine a room of three or four women – or 20-25 women – the numbers don’t matter – just picture a small group of women suddenly piecing together a family history that reveals the toll that birth control has taken on their mothers, sisters, nieces, and cousins.
Now THAT would be an honest discussion that could liberate and empower an entire group of women at once.
For more information about the history of hormonal birth control:

The FDA approved The Pill despite it not being proven safe. Today, it has been linked to everything from blood clots and cancer to lupus and Crohn’s disease — and still has not been proven safe.
This book explores the medical and historical disconnects that brought us to this point.
Last updated on October 21, 2023 at 9:38 pm – Image source: Amazon Affiliate Program. All statements without guarantee.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.


















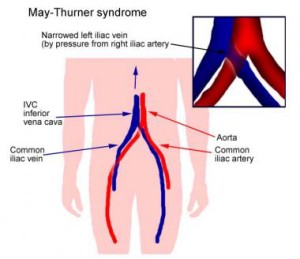 Most do not know this until they end up in the hospital with a blood clot. For these women, the risk for deep vein thrombosis, particularly in the left leg is even higher, especially on birth control (most especially, I believe, though this is pure speculation, when using a cervical ring like the NuvaRing). Again, add long sit times, an injury perhaps, and we can begin to see how the risk for blood clots in the female athlete using hormonal contraception can be much higher than for her teammates who do not use hormonal contraceptives.
Most do not know this until they end up in the hospital with a blood clot. For these women, the risk for deep vein thrombosis, particularly in the left leg is even higher, especially on birth control (most especially, I believe, though this is pure speculation, when using a cervical ring like the NuvaRing). Again, add long sit times, an injury perhaps, and we can begin to see how the risk for blood clots in the female athlete using hormonal contraception can be much higher than for her teammates who do not use hormonal contraceptives.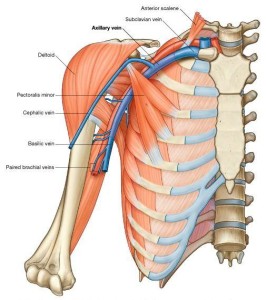 It is believed that the repetitive trauma that these sports require imposes strain on the subclavian vein leading to microtrauma of the endothelium and activation of the coagulation cascade. This alone is a risk factor for developing a blood clot, but when we add a few more variables, an intense competition, dehydration, a long flight home with upper body immobility and perhaps compression (sleeping on one’s arm), and enter these variables into an system primed for coagulation by hormonal birth control, the risk for dangerous blood clots increases significantly.
It is believed that the repetitive trauma that these sports require imposes strain on the subclavian vein leading to microtrauma of the endothelium and activation of the coagulation cascade. This alone is a risk factor for developing a blood clot, but when we add a few more variables, an intense competition, dehydration, a long flight home with upper body immobility and perhaps compression (sleeping on one’s arm), and enter these variables into an system primed for coagulation by hormonal birth control, the risk for dangerous blood clots increases significantly.