I recently became aware of a case of a boy who had died from a myocarditis and subsequent heart failure after he had received the Gardasil vaccination. He was reportedly completely healthy before the vaccination and the death had been directly attributed to it. The autopsy report was very striking. Examination of heart muscle had revealed a “long narrow band of dark reddish discoloration, somewhat darker than the rest of the myocardium”. Although this was not described more fully, it strongly suggested that the description was that known in medical jargon as “ragged red fibers”.
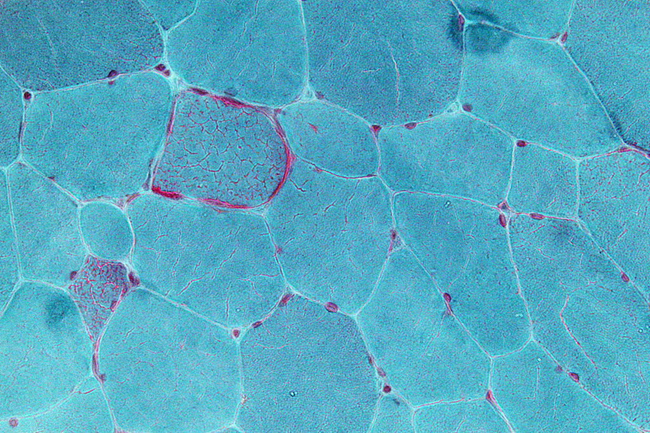
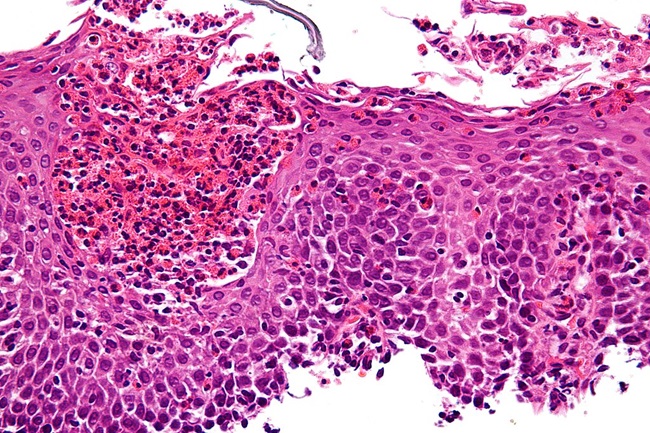
Ragged red fibers are commonly seen with mitochondrial dysfunction in muscle tissue. The ragged red fibers indicate an accumulation of abnormally functioning mitochondria in the muscle tissue. Though ragged red fibers have been studied extensively in individuals with inherited mitochondrial disease, it is not clear whether this type of damage can be acquired or induced in individuals with or even without mtDNA mutations. Studies in rats, however, have shown that thiamine deficiency does result in the finding of ragged red fibers in muscle tissue, suggesting that this damage can be induced. In view of the many posts on this website discussing the association of thiamine deficiency with Gardasil vaccination, I became very interested and began to search the literature for what was known about the relationship of thiamine with ragged red fibers.
Mitochondria
Before I offer an explanation, let me remind the reader about mitochondria. We have between 70 and 100 trillion cells that make up the human body. Each cell has a prescribed function and each of the body organs consist of highly specialized cells. What we tend to forget is that our food provides the fuel from which energy is generated. To use a simple analogy, a car without an engine would not be capable of functioning. Mitochondria are the “engines” that exist in each one of those cells. They provide the energy for which function is dependent. We inherit from our parents thousands of genes that control how we look, behave and perform as personalities. These are known as cellular genes, but mitochondria have entirely separate genes inherited only from the mother. They control the mechanisms of the “engines” (mitochondria) in generating energy. Disease can be caused by genetic mutations in cellular genes but in the past decade it has been recognized that mitochondrial genes can be responsible for disease and more than 50 different mutations have been described. The majority of these mutations are single base changes in the DNA strand. They do not necessarily produce disease by themselves. Other factors related to nutrition, lifestyle, and as I suspect, medications and vaccines, may have to come into play.
To express this fully, a deficiency of thiamine (or other vitamins) can be so mild that the symptoms, if any, are regarded as inconsequential or ascribed to other causes. This obviously becomes more important if there is an associated unknown genetic risk that affects the metabolism of the vitamin. Because thiamine is so vital to energy synthesis, the imposition of a stress factor such as a mild infection or an inoculation can precipitate more severe symptoms. Meeting stress requires adaptive energy. To provide an analogy, a car with an inefficient engine may be adequate on the level but be inadequate to meet the stress of climbing a hill.
Mitochondrial Disorders are Multi-Systemic
I should note that mitochondrial disorders are often multi-systemic due to impaired oxidation that results in defective mitochondrial energy production. That means there can be symptoms from damage to multiple organ systems simultaneously. Mitochondrial disorders are also phenotypically different amongst family members with the same mutation and amongst individuals with acquired mitochondrial dysfunction. In other words, how mitochondrial disorders or damage can present symptomatically varies radically from person to person. This variation is what makes diagnosing mitochondrial dysfunction difficult for many practitioners. The symptoms don’t always fit into nice, neat, discrete diagnostic categories that so many of us are accustomed too. This variability in mitochondrial dysfunction makes it difficult to attribute the action of a vaccine or medication as the cause of a subsequent illness, or in some cases, death. How is it possible for a medication or vaccine to induce so many seemingly disparate symptoms? To answer that question, we need to understand a few mechanisms.
Thiamine Deficiency Post Gardasil
Over the last several years, we have identified several cases of laboratory confirmed thiamine deficiency post Gardasil. Additionally, when lab testing was unavailable (few labs offer the appropriate assays for thiamine testing), clinical response to thiamine treatment has been confirmatory. In more recent research, we have identified thiamine transporter gene mutations (SLC19A2) in a group of young women who experienced severe reactions to the Gardasil vaccine (reported within this article). Combined, this suggests that thiamine deficiency is involved in some of the adverse reactions observed and that the potential danger from the use of a vaccine requires more information from the patient and his/her family. How can something as simple as thiamine cause so many adverse reactions and even death? And can a medication or vaccine induce thiamine deficiency?
Thiamine is Critical for Mitochondrial Functioning
Thiamine is a critical co-factor in multiple pathways involved in mitochondrial energy production (ATP). It is necessary for carbohydrate processing via the pyruvate pathway and it is necessary for fatty acid processing because of its involvement with the HACL1 enzyme. In other words, the mitochondria depend upon thiamine to function. Diminish thiamine and all sorts of compensatory reactions are initiated which, if not stopped, can cause death. Thiamine deficiency in adults, particularly those with chronic alcoholism, is considered a medical emergency. It has not, however, been readily recognized in reference to other causes of malnutrition where there is an imbalance between the ingested calories and the necessary vitamins – high calorie malnutrition. This particularly applies to thiamine.
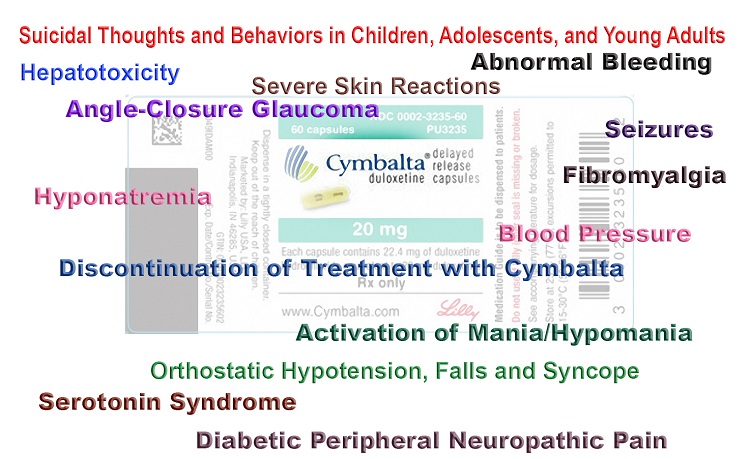
The Gardasil Thiamine Relationship
There are multiple mechanisms by which a vaccine or medication can induce thiamine deficiency or push an existing or subclinical deficiency into a danger zone. Beginning with the later first, the modern western diet is replete with highly processed foods that are dense in calories but lack non-caloric nutrients. It is entirely likely that many individuals, even those that appear healthy, are borderline thiamine deficient or intermittently thiamine deficient when stressors or illnesses arise. Vaccines are toxicological stressors to the immune system and broadly speaking, any stressor, but particularly one that demands an immune reaction like a vaccine, is capable of inducing a thiamine deficient state. In individuals with latent errors in thiamine absorption (GI disorders), distribution or metabolism (like those with thiamine transporter mutations), or anything that evokes even a slight degradation in thiamine nutrient availability, thiamine deficiency will be exacerbated exponentially.
The Gardasil vaccine was developed using a yeast type base*. The yeast produces an enzyme called thiaminase that inactivates thiamine. Again, against the backdrop of poor diet or diet high in foods that also produce thiaminase (coffee, tea, certain fish), but especially, against the backdrop of a genetic or acquired mitochondrial issue recognized or latent, the reaction to the vaccine (or medication, as many medications can block thiamine directly or indirectly), can be devastating.
Finally, vaccines, because of the adjuvant carriers like aluminum, damage to mitochondrial functioning more broadly, with both structural and functional changes are noted. Damaged mitochondria are not only less capable of producing appropriate amounts of cellular energy but are also incapable of performing the myriad of other functions with which the mitochondria are tasked.
Ragged Red Fibers and Cardiomyopathy
Let us continue with this case and the ragged red fibers observed in the myocardium, the heart muscle, of the deceased boy. For those who study mitochondrial disorders, one of the more common histological hallmarks of the disease process in mitochondrial disorders are ragged red fibers. These are muscle fibers with abnormal focal accumulations of mitochondria. According to the coroner’s report:
“a long narrow band of dark reddish discoloration which is somewhat darker than the rest of the myocardium, extends over a length of 6 cm and has a width of 0.4 cm extending from the anterior base of the heart almost to the apex. ..this lesion is limited to the anterior free wall”
was observed. The coroner concluded that the boy developed asymptomatic myocarditis in weeks preceding his death. The myocarditis evoked a heart attack which was the determined cause of death. A subsequent review by a medical expert hired by the attorneys presenting the case against the vaccine manufacturer, went a little deeper, attributing the dark fibers to a vaccine-induced inflammatory reaction resulting from the first dose of Gardasil. He argued that the first dose of the vaccine initiated a heart attack that was somehow not noticed by the child, as he continued to play football. Upon receiving the second dose, however, the damage initiated by the first dose was exacerbated, slowing heart function until it failed entirely. In either case, the heart muscle was irreparably damaged such that the child died in his sleep with the Gardasil as the causal agent.
Given my background in thiamine research, and thiamine’s role in heart function (as well as in brain function), I immediately wondered if the observed “band of darkish reddish discolorations” could be the ragged red fibers so common in mitochondrial dysfunction and if there presence indicated thiamine deficiency. Furthermore, I suspected that the fact that he died in his sleep strongly suggested that the automatic respiratory mechanism governed by the brain stem was implicated. This too, is a strong support for thiamine deficiency. I should note, I did not have access to the full report; only that which was published online.
Thiamine Deficiency and Ragged Red Fibers: Experimental Evidence
As I have argued previously and elaborated above, the HPV vaccines can induce and/or exacerbate thiamine deficiency. The question is whether thiamine deficiency can induce ragged red fibers in muscle.
To that end, I discovered a manuscript in the Archives of Neurology: Neuropathic and mitochondrial changes induced in rat muscle, showing that experimentally in rodents this was possible. Thiamine deficiency could induce ragged red fibers in muscle tissue. In this particular study, two groups of rats were compared. One group was fed a normal diet and the other group was fed a diet deficient in thiamine. The rats with thiamine deficient diets developed ragged red fibers in the muscles. Other abnormalities were described not found in the muscles of the control rats. The authors concluded that thiamine deficiency was responsible for the observed ragged red fibers and may be involved in what are now called the “ragged-red diseases”.
Case Studies: Ragged Red Fibers, Thiamine and Mitochondrial Disease
Japanese investigators studied two siblings with muscle disease due to mitochondrial dysfunction, a mutation in the mitochondrial DNA, and familial thiamine deficiency. Ragged red fibers were found in muscle biopsies. The older brother had presented at the age of 20 years when he developed muscle disease and beriberi heart disease. Thiamine deficiency was present in the siblings and parents and ragged red fibers were noted in muscle biopsies from the siblings. The development of symptoms at the age of 20 years certainly indicates that it was not a purely genetically determined disease.
Another article in a Japanese journal reported a nine year-old boy with muscle and brain disease in whom thiamine administration gave temporary improvement. A muscle biopsy had revealed numerous ragged-red fibers.
Mitochondrial diseases have a special predilection to involve the brain in view of its high metabolic demand. Patients with a form of disease known as myoclonic epilepsy have ragged red fibers in muscle tissue thus identifying the underlying mitochondrial cause.
Mitochondrial Dysfunction in Myocardial Infarction and Sudden Death
In a recent review of mitochondrial cardiomyopathies we see some striking similarities between this case and what has been recently recognized. Accordingly:
The presentation of mitochondrial cardiomyopathy includes hypertrophic, dilated, and left ventricular (LV) noncompaction, and the severity can range from no symptoms to devastating multisystemic disease. Severe cardiac manifestations include heart failure and ventricular tachyarrhythmia—which can worsen acutely during a metabolic crisis —and sudden cardiac death. Mitochondrial crisis is often precipitated by physiologic stressors such as febrile illness or surgery [a vaccine] and can be accompanied by acute heart failure.
Bioenergetic derangements are increasingly recognized as major culprits in the development of cardiac hypertrophy and in the progression to heart failure, in both acquired and inherited disease. The mitochondria are a crucial platform for energy transduction, signaling, and cell-death pathways that are broadly relevant to heart failure, even in the absence of an underlying mitochondrial myopathy. Oxidative stress and mitochondrial dysfunction are key factors in the development of most heart failure.
Connecting the Dots
The question remains, how could this boy’s death from a vaccination have been predicted and thus avoided? It is clear that there was temporal relationship between the vaccine, the damage to his heart, and his subsequent death. Mechanistically, the evidence is collaborative with this association. From an evidentiary standpoint, the vaccine appears capable of inducing mitochondrial dysfunction via its ability to diminish thiamine, and likely, via other, yet to be identified, mechanisms. Of key importance, however, is that thiamine depletion on its own, can induce ragged red fibers in muscle tissue, probably including the heart muscle. When the vaccine is given to an individual with genetic or other risk factors (like comorbid health issues, poor diet, and/or the high metabolic demands of sports training), the results can be devastating. Given that this combination of variables includes most teenagers, it is difficult not to see the dangers of this vaccine. In conclusion, if the long band of dark reddish muscle tissue described in the heart muscle of the boy had been shown to be ragged red fibers, it would have supported mitochondrial dysfunction as the cause of death.
*It should be noted that the Cervarix HPV vaccine was not developed using a yeast base, and thus, it is not clear by what mechanism(s) it might diminish thiamine concentrations.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image: Very high magnification micrograph showing ragged red fibres (also ragged red fibers), commonly abbreviated RRF, in a mitochondrial myopathy. Gomori trichrome stain.
Nephron, CC BY-SA 3.0, via Wikimedia Commons
This article was published originally on Hormones Matter on January 5, 2016.