Over the last several months, the writers and researchers at Hormones Matter have posted a number of articles about mitochondrial dysfunction and thiamine deficiency. Thiamin, or thiamine as the internet search engines prefer, is critical to mitochondrial function. We’ve learned that thiamine deficiency can emerge gradually due to dietary inadequacies or more suddenly as a result of a medication, environmental or surgical insult. Regardless of the cause, deficits in thiamine evoke devastating health issues that can be treated easily if identified. More often than not, however, thiamine deficiency is not assessed and symptoms are left to escalate, mitochondrial damage increases, and patient suffering continues. Because thiamine deficiency is rarely considered in the modern scientific era, mild symptoms are ascribed to other causes such as “an allergy” or “it’s all in the patient’s head”. If, however, the cause is not revealed, the same old dietary habits will continue and can be guaranteed to produce much more severe and difficult to treat chronic disease.
Although there are a myriad reasons why mitochondria are damaged, medication or vaccine reactions paired with latent nutritional deficiencies seem to be common. Predicting who and how the mitochondrial dysfunction might appear, however, is more complicated. Quite often, athletes and individuals considered healthy are hit harder by a stress factor such as a vaccine than those whom we might not regard as particularly healthy. There are several potential reasons for this, some of which have been outlined previously. In this post, I would like to add one more reason why highly active, high performing individuals might be hit harder and more quickly than their less active counterparts with vaccine or medication reactions that induce thiamine deficiency.
Mitochondria are the Engines of the Cell
To use an analogy, the usefulness of a car obviously depends upon its engine. Mitochondria are the “engines” of each cell within our bodies, all 70 to 100 trillion cells that make up an adult body. They are known as organelles and are so small that their structure can only be seen with an electron microscope. But we can take this analogy further by comparing each cell to a different car model. A high powered car uses more gasoline than a low powered one and there are many models of each type of car. So some cells in the body require more energy than others, depending on the special function of the cell. The most energy consuming cells are in the brain, the nervous system and the heart, followed by the gastrointestinal system and muscles. That is why those organs and tissues are most affected in the disease known as beriberi, the thiamine deficiency disease that we have discussed previously in other posts. The function of other organs is affected by the deficiency because of the changes in the control mechanisms originating in the brain through the autonomic (automatic) nervous system.
It has been pointed out that this disease in its early stages affects the autonomic nervous system by causing POTS. Beriberi and POTS, both being examples of dysautonomia (abnormal activity of the autonomic nervous system), can only be distinguished by finding evidence of thiamine or other nutrient deficiency as a cause. Thiamine is but one factor whose deficiency causes loss of cellular energy, resulting in defective brain metabolism and dysautonomia. Although the relationship with vaccination is conjectural, some individuals with post Gardasil POTS were found to be thiamine deficient and had some relief of symptoms by taking supplementary fat soluble thiamine, an important derivative that occurs in garlic and has been synthesized. Not all of these thiamine deficient individuals have benefited to the same degree, suggesting that other deficiencies might also be involved. This post is to provide some information about more recent knowledge concerning the action of thiamine and the incredible, far-reaching effects of its deficiency, particularly in the brain. Experimental work in animals has shown that thiamine deficiency will damage mitochondria, a devastating effect for an acquired rather than a genetic cause. Far too much research has been devoted to genetic cause without sufficient attention to the way genes are influenced by diet and lifestyle.
The Importance of Enzymes to Mitochondrial Function
Before I provide this new information, let me remind the reader that enzymes, like cogwheels in a man-made machine, enable bodily function to occur. The importance of thiamine is that it is a cofactor to many of the enzymes that preside over energy metabolism. Without its cofactor an enzyme becomes inefficient. Perhaps it might be compared with missing teeth in a cog wheel. With missing teeth the cog wheel may still function but not nearly as well as it would with all of its component parts.
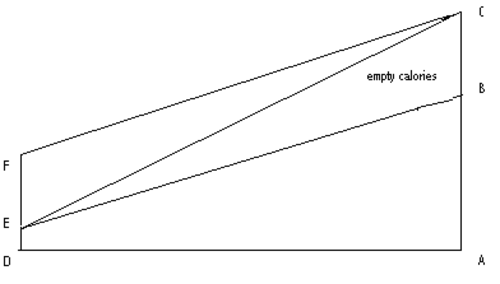
In previous posts we have discussed how thiamine deficiency can be caused by an excess of sugar in the diet. I have likened this to a “choked engine” in a car where an excess of gasoline, relative to insufficient oxygen concentration in the mixture, makes ignition of the gasoline extremely inefficient. Bad diet, one that is rich in sugary, carbohydrate laden foods may be one of the more common contributors to latent thiamine deficiencies. Excessive intake of processed fats and the concomitant changes to mitochondrial function and energy metabolism may be another important contributor.
Thiamine and Fat Metabolism
All the enzymes affected by thiamine deficiency have a vital part to play in obtaining cellular energy from food by the process of oxidation. Most of them have been known for many years but in the nineties a new enzyme was discovered. It has a very fancy name that has been simplified by calling it HACL1. Only in recent years has it been found that HACL1 is dependent on thiamine as its cofactor. Although not reported, it may mean that it is also dependent on magnesium. This is exceedingly important because it introduces the fact that thiamine is involved in fat as well as carbohydrate metabolism, something brand new, even to biochemists.
Here I must digress again to describe another type of organelle called a peroxisome that occurs in our cells. Like mitochondria, they are infinitesimally small. Their job is to break down fatty acids and they have a double purpose. One purpose is to synthesize very important substances that construct and maintain cells and their function: they are particularly important in the brain. The other purpose is what might be called fuel preparation. As the fatty acids, consisting of long carbon chains, are broken down, the resulting smaller fragments can be used by mitochondria as fuel to produce energy. Failure to break down these fatty acids can result in the accumulation of natural components that may be toxic in the brain and nervous system or simply result in lack of one type of fuel. That is why feeding medium chain triglycerides by administration of coconut oil has been reported useful to treat early Alzheimer disease. They can be oxidized in mitochondria.
The Important Use of Fatty Acids in Mitochondrial Health
Here, I want to use another analogy. Imagine a lake that admits water to a river through a sluice gate that has to be opened and closed by a farmer who regulates the supply of water. If the gate is open the river will supply water to the surrounding fields. If however the gate is closed, the river will begin to dry up and the crops in the fields will suffer. Perhaps the farmer half closed the gate during a rainy period and has forgotten to open it when a dry period follows. High temperatures in the dry period results in insufficient water to meet the growth needs of the crops.
In this analogy, the lake represents food, the sluice gate is the HACL1 enzyme and the farmer who controls the gate represents thiamine. The water in the river represents the flow of fatty acids to the tissues for the double purpose of cellular construction and fuel for oxidation. The half open gate represents a minor thiamine deficiency, more or less sufficient for everyday life but not enough when there is greater demand. A high temperature that increases the water needs for crops represents Gardasil and many other medications as a stress factor, placing a greater demand on essential metabolic action. The analogy also implicates the nature of the crops, some of which require more water than others. The crops, of course, represent body tissues and organs.
If we consider high performing individuals, whether academically or athletically, like high performance cars or crops that demand more nutrients, we can see how a previously unrecognized minor deficiency might trigger clinical disease by the stressful demands of a vaccine or medication. Some pharmaceuticals can attack thiamine directly, like Gardasil and the fluoroquinolones, while others attack different pathways within the mitochondria.
No matter the pathway, high performing individuals, with high energy needs not covered by diet, may be hit harder when a medication attacks mitochondrial energy.
The Outcome of Defective Fatty Acid Metabolism
Returning back to the HACL1 enzyme, we now know that HACL1 is the first thiamine dependent enzyme to be discovered in peroxisomes. It is research news of the highest importance, affecting us all. Its action is to oxidize a diet related fatty acid called phytanic acid and fatty acids with long carbon chains that cannot be used for fuel until they are broken down. Phytanic acid is obtained through consumption of dairy products, ruminant animal fats and some fish. People who consume meat have higher plasma phytanic acid concentrations than vegans. If the action of HACL1 is impaired because of thiamine deficiency the concentration of phytanic acid will be increased. The river in the analogy actually represents a series of enzymatic reactions that may be thought of as down-stream effects, whereas thiamine deficiency, being up-stream, affects all down-stream phenomena. One of the reasons thiamine deficiency is such an important contributor to illness is because its effects are broad.
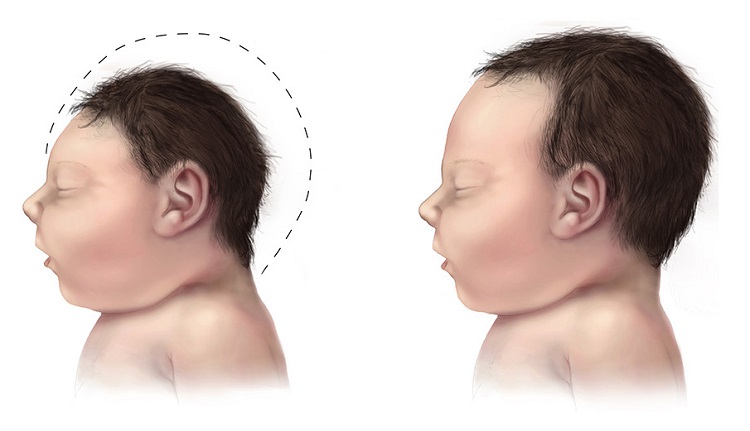
These enzymatic reactions, known technically as alpha oxidation, involve four separate stages. It has been known for some time that if another enzyme at stage two is missing because of a gene defect, the result will be damage to the neurological system known as Refsum’s disease. Symptoms include cerebellar ataxia (also reported after Gardasil vaccination), scaly skin eruptions, difficulty in hearing, cataracts and night blindness. Other genetic mutations in alpha oxidation, resulting in various biochemical effects, result in a whole variety of different diseases. This places thiamine deficiency as a potential cause for all the down-stream effects resulting from defective alpha oxidation, for it has been shown in mice that this vitally important chemistry is totally dependent on presence of thiamine. Since its complete absence would be lethal, we have to assume that it is mild to moderate deficiency, equivalent to a partial closure of the sluice gate in the analogy.
Sources of Phytanic Acid: How Diet Affects Thiamine
In ruminant animals, our source of beef, the gut fermentation of consumed plant materials liberates phytol, a constituent of chlorophyll, which is then converted to phytanic acid and stored in fat. The major source of phytol in our diet is, however, milk and dairy products. It raises several important questions. If thiamine deficiency is capable of causing an increase in phytanic acid in blood and urine, it might be a means of depicting such a deficiency in a patient with confusing symptoms. It might also explain why some individuals who have been shown to have thiamine deficiency by means of an abnormal transketolase test have symptoms that are not traditionally accepted as those of such a deficiency, perhaps because of loss of efficiency in HACL1.
If an excess of sugar in the diet gives rise to a secondary (relative) thiamine deficiency, we are provided with an excellent view of the extraordinary danger of empty simple carbohydrate and fat calories, perhaps explaining much widespread illness in Western civilization. Interestingly, it would also suggest that something as benign as milk could give rise to abnormal brain action in the presence of thiamine deficiency, because of phytanic acid accumulation. Our problems with dairy products may go well beyond lactose intolerance and immune dysregulation.
In sum, the discovery of HCAL1 enzyme and its dependence upon thiamine suggests one more mechanism by which thiamine deficiency affects mitochondrial functioning. As emerging evidence indicates a myriad of environmental and pharmaceutical insults impair mitochondrial functioning, thiamine deficiency ought to be considered of prime importance. Deficits in thiamine evoke devastating health issues that can be treated easily if identified. If, however, thiamine deficiency is not identified and the same old dietary habits continue, the latent thiamine deficiency can be guaranteed to produce a much more severe and difficult to treat chronic disease. Moreover, individuals with thiamine deficiency who do not respond sufficiently to thiamine replacement might also have aberrant fatty acid metabolism. This too should be investigated and dietary changes adopted.