I couldn’t help noticing the Wall Street Journal of Thursday, June 7, in which a column reported a completely unexpected suicide. The title of the column was “Kate Spade’s Family Recounts Her Battle With Depression”. It was reported that “Ms. Spade had suffered from depression and anxiety, and was being treated with medication and therapy. Depression and anxiety disorders occur simultaneously in about 25% of general practice patients. In the abstract, the author says “about 85% of patients with depression have anxiety and 90% of patients with anxiety have depression. Benzodiazepines may help alleviate insomnia and anxiety but not depression”. It must be obvious that the general impression is that these are two different expressions of psychological disarray that require different drugs to treat them. Evidently, Ms. Spade had left a suicide note indicating that she had been under mental stress from her marriage. There were other stresses reported. She had been living separately from her husband for 10 months and had been seeking help for the past five years.
The incongruity requires explanation. Here was a 55-year-old woman who was highly successful in the eyes of the world and her suicide appears to be completely incongruous, as indeed most suicides are. There should be a logical explanation for such an anachronism. The instinct for life is incredibly strong for us and indeed for all creatures in the animal kingdom. I offer my explanation here, based on the contention that the human brain is an electrochemical machine and that its functions are highly dependent on an adequate supply of energy. This does not take into account the concept of a soul that must remain one of the great mysteries of life.
Revisiting Freud: The Ego and the Id
According to Sigmund Freud, the id is the subconscious mind supervised by the ego and what he called the super-ego. All are built upon the presupposed existence of conscious and unconscious thoughts. Modern research has failed to find individual areas in the human brain dealing with the control of specific action. Its function is now regarded as an integrated organ, all parts of which share that action. However, much of this activity is entirely automatic and below conscious level. All brains in higher members of the animal kingdom are built on the same anatomical principle, presumably reflecting a “oneness” in design. If we are to accept evolution as the driving force, the brain of each animal has been developed to service that animal in its natural niche. The niche of Homo sapiens appears to be that of the dominant species and it has evolved from a more primitive state to a more sophisticated one, gradually introducing increased complexity. Brain action would be expected to become more and more sophisticated over time, perhaps making us more cooperative.
We have no idea what is in store for us with continued evolution, but it has long seemed to me that we are still relatively primitive at the philosophical level. Under stressful conditions, the actions of the human brain are much less predictable. However we consider the distribution of brain function, it is an electrochemical machine and a great deal of its activity is unconscious and purely automatic. Body organs signal the brain that then gives instructions to them via the autonomic and endocrine systems. It is therefore convenient to accept the ego and the id, each with its separate functions, however, they are controlled, by the conscious and unconscious mind. Some of the net behavior might be perceived as actions of the automatic component, governed and permitted by the conscious component. It has been suggested that human beings are built as “mean fighting machines equipped for self-interest”.
The Nervous System
Many posts on this website describe the difference between the so-called voluntary and the autonomic nervous systems. The term “voluntary” indicates that we can think and move at will and its actions are dictated by the conscious mind. The autonomic nervous system is almost completely automatic and governs many purely reflex actions, the fight-or-flight reflex being the best known. Hunger and thirst are self-preservatives. The sex drive preserves the continued existence of the species. Yes, these reflexes give us a sense of pleasure, which is the driving incentive and the brain provides us with sensory mechanisms that provide that pleasure. Everything is tied together by a complex code known as DNA, whose individual characteristics describe the physical profile and personality of each animal including humans. From a purely philosophical point of view, it calls into question whether we truly have free will or whether we are programmed by the environment in which we find ourselves. If all components fit together as designed, we can say that the “blueprint” for each person dictates the nature of the personality and reflects his/her mental and physical health. Our training to meet life starts in infancy and is in the hands of parents.
Of Stress and Stressors
Stress is a physical or mental event to which each of us has to adapt. As I have mentioned in other posts on this website, a Canadian researcher by the name of Hans Selye studied the effect of physical stress in animals for many years. He came to the conclusion that virtually any form of stress demanded an increase in the supply of cellular energy, much like the engine of a car climbing a hill. A stressed animal had to adapt to the injuries applied by Selye. He called it the “General Adaptation Syndrome”. He used many different methods to induce stress because he wondered whether there were different responses, depending on the nature of the stressor. He found that the stress response was uniformly identical across species and was able to divide the General Adaptation Syndrome into several predictable phases, each of which was repeatable in each experiment. Not surprisingly, his studies included an array of sequential biochemical changes in the body fluids. I found these changes to be similar to the laboratory changes seen in chronically sick patients. One of his students was able to produce the syndrome by first making the animal deficient in the vitamin thiamine, thus supporting the role of energy deficiency as the causative factor. Selye suggested that human health broke down as a result of energy failure, particularly in the brain, leading to what he called “the diseases of adaptation”. It is probably true that some form of life stress is absolutely necessary for a person to contemplate suicide. Therefore, it seems necessary to discuss the mechanisms by which the brain responds to stress.
The Biological Brain
Whether we like to recognize it or not, the brain is an electrochemical machine whose functions, like any machine, require energy. The fact that the brain requires 20% of the total oxygen inhaled is an absolute indication of its energy requirement. There is much evidence that even a mild reduction influences brain activity and this will be reflected in some kind of change in thought processes and the consequent behavior resulting from it. Nutrition affects mood. A deficiency of many vitamins is associated with psychological symptoms. In some elderly patients, folate deficiency is associated with depression. Iron deficiency is associated with apathy, depression, and rapid fatigue when exercising. In several studies, an improvement in thiamine status was associated with improved mood. One of the major manifestations of obstructive sleep apnea is profound and repeated (episodic) hypoxia (insufficient oxygen) during sleep. This increase in activity in the sympathetic nervous system affects blood pressure. Thiamine deficiency induces gene expression similar to that observed in hypoxia and has been referred to as causing pseudo-hypoxia. Magnesium and thiamine deficiency have both been implicated in depression.
Hypoxia and Pseudohypoxia in Depression and Anxiety
During many years of medical practice, I found that a mild degree of thiamine deficiency was responsible for symptoms that are often regarded as psychological. Chronic anxiety and depression were regularly alleviated by getting people to understand the importance of an appropriate diet, together with the administration of supplementary vitamins, the most important of which were thiamine and magnesium. I could never understand how a patient could be actually blamed for producing symptoms beyond the comprehension of the physician. Abnormal thoughts, emotions, and all forms of mental activity are produced by electrochemical reactions that are exaggerated by a mild degree of hypoxia or pseudo-hypoxia.
Anxiety and depression are perfectly normal emotional reactions but when they are sustained for absolutely no reason, it is because of this biochemically initiated exaggeration. In particular, the sympathetic branch of the autonomic nervous system is easily activated because any degree of oxygen lack is obviously dangerous to the organism and a fight-or-flight reflex reaction would be initiated by the perception of danger. This reflex, because of its nature, might give rise to aggressive behavior when a nursed a grievance explodes into violence. The widespread intake of empty calories, particularly in the form of sugary and fatty substances, is responsible for polysymptomatic disease in millions. Such individuals cannot handle the normal stresses of life and are much more easily imbued with a sense of hopelessness. Suicide seems to be the only option. The idea that dietary excesses might be responsible for depression and suicidal ideation is not a presently acceptable concept, but the biochemical results of alcohol and sugar ingestion are identical in the part of the brain that has to deal with these inbuilt vital reflexes.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
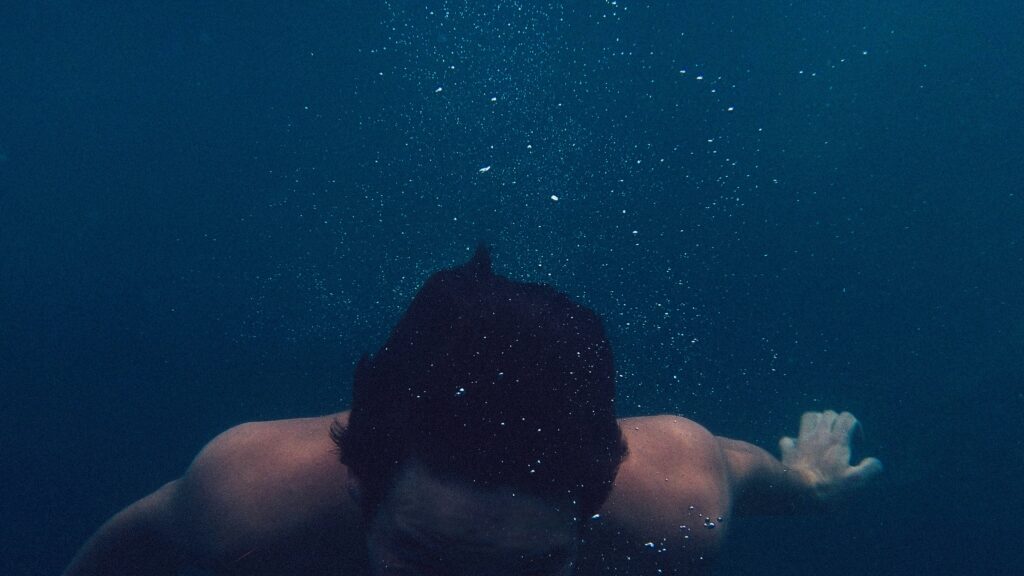
Photo by Jacob Walti on Unsplash.
This article was published originally on June 20, 2018.