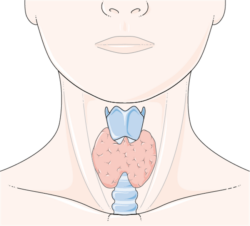
One in five women of reproductive age suffers from some form of thyroid disease, mostly hypothyroidism (Gharib et al. 2005; Hollowell et al. 2002). In adult women, 95% of clinical hypothyroidism results from primary disease of the thyroid gland, generally, the autoimmune condition Hashimoto thyroiditis (Wartofsky et al., 2006). Autoimmune thyroid disease is also common among women with Type 1 diabetes mellitus, Sjogren syndrome, Addison disease, or pernicious anemia. Up to 25% of patients with Type 1 diabetes will develop postpartum thyroid disease (Alvarez-Marfany et al., 1994).
Hypothyroidism During Pregnancy
What happens when a woman with untreated thyroid disease gets pregnant? Depending upon the diagnostic criteria, hypothyroidism affects 0.3% (Casey & Leveno, 2006) to 5% (Gharib et al. 2005) of pregnancies. The symptoms are vague and are similar to other pregnancy concerns making diagnoses based on clinical symptoms alone difficult. Hypothyroid symptoms include fatigue, constipation, cold intolerance, muscle cramps, insomnia, weight gain, carpal tunnel syndrome, hair loss, voice changes, and slowed thinking.
The consequences of undiagnosed hypothyroidism during pregnancy are significant. Hypothyroidism is associated with premature birth, pre-eclampsia, abruption, low birth weight (LBW), postpartum hemorrhage, and impaired neuropsychological development in childhood (Burman, 2009). Research found that fetal loss was higher in untreated hypothyroid women (29%) vs hypothyroid women taking levothyroxine (6%), highlighting the need for early detection (Hallengren 2009).
Hyperthyroidism During Pregnancy
Hyperthyroidism, the result of an excess of thyroid hormones, complicates less than 1% of pregnancies (ACOG Practice Bulletin, 2002). Symptoms of hyperthyroidism are uncommon in normal pregnancy and thus somewhat easier to identify clinically. Maternal symptoms include weight loss or failed weight gain despite increased dietary intake, resting tachycardia, hypertension, tremor, eye stare, eyelid lag, proptosis, and thyroid enlargement or nodule.
Graves’ disease, an autoimmune disorder occurring in 0.5% of the population, accounts for more than 90% of the hyperthyroidism associated with pregnancy. Complications associated with undiagnosed or poorly managed hyperthyroidism during pregnancy include pre-term labor, pre-eclampsia and maternal thyroid storm, fetal tachycardia, low birth weight, congenital abnormalities, and stillbirth.
Should Pregnant Women Be Tested for Thyroid Disease?
Yes, but there is little consensus among the major medical associations regarding who, when, and how to test for thyroid function during pregnancy. It is argued that by the time TSH (the gold standard in thyroid diagnostics) becomes hyper-elevated and the clinical symptoms emerge, the damage to fetal neurodevelopment related to insufficient maternal T4 stores, has already been done (Calvo et al. 2002). Emerging evidence suggests that maternal T4 levels may not track directly with elevated TSH levels especially in the first trimester when the demands for maternal T4 are greatest (Morreale de Escobar et al. 2000), making the need for more advanced testing techniques even more important.
Iodine Deficiency and Hypothyroidism: One More Factor to Consider
Complicating matters even further, in iodine-deficient populations, neither TSH, T4 nor T3 denote the underlying deficiency, which as it progresses, inevitably elicits the range of fetal developmental issues and maternal complications associated with hypothyroidism. In the US, approximately 10% of the population is iodine deficient while 50% of Europe is iodine deficient (Zimmerman 2009). In recent years, iodine deficiency has increased in the US in women of reproductive age with 14.9% percent potentially iodine deficient (Hollowell et al. 1998). Similarly, the incidence of congenital hypothyroidism in newborns has also increased in the US over the last two decades (Parks et al. 2010).
Iodine deficiency in women can lead to overt hypothyroidism and consequent anovulation, infertility, gestational hypertension, spontaneous first-trimester abortion, and stillbirth (DeLong et al., 1997). Iodine deficiency is also associated with an increased risk for thyroid carcinoma in animal models and humans (Mellemgaard et al., 1998). In the Bryansk region of Russia, an area of known radioactive I-131 exposure following the Chernobyl disaster, the risk of all types of thyroid cancer was inversely associated with urinary iodine excretion levels (WHO Health Risk Assessment).
What Constitutes Hypothyroidism in Pregnant Women?
In addition to the debate over whether to test pregnant moms routinely for thyroid disease, especially hypothyroid moms, there is much debate regarding what constitutes elevated TSH and whether to include subclinical hypothyroidism (SCH) or mild hypothyroid cases in the testing matrix (Fatourechi 2009; Surks et al. 2004). SCH or mild hypothyroidism is suggested by only slightly elevated TSH concentrations without the normally accompanying changes in T4. Arguments against testing for SCH include the enormous increase in cases; up to 28 million more people could be diagnosed with hypothyroidism, and the conflicting data regarding treatment benefits and disease progression. Moreover, recent evidence suggests significant age and race-based differences in TSH reference ranges across the non-pregnant population complicating diagnoses even further (Surks & Boucai 2010).
Given the dire consequences of untreated thyroid dysfunction during pregnancy, there is a need for more accurate, non-invasive and less expensive thyroid function tests with reference ranges specifically identified for this population of women. Screening for thyroid function in women of reproductive age and in pregnant women could reduce maternal and fetal complications.
Our view on thyroid disorders during pregnancy can be summarized as follows:
- Thyroid disease is common in pregnancy.
- Hypothyroidism and hyperthyroidism are associated with adverse pregnancy outcomes, and treatment may improve these outcomes.
- Untreated hypothyroidism during pregnancy is associated with impaired intellectual development in childhood.
- Routine, universal screening for thyroid function in women of reproductive age and in pregnant women could reduce could reduce maternal and fetal complications
- Normal reference ranges for thyroid function tests in pregnancy must be established
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Postscript: This article was originally published on February 21, 2012 and updated on July 11, 2014. If I were to rewrite this post now, I would attribute much of the thyroid dysfunction to nutrient deficiencies.