A paper published in Science Translational Medicine, provides preliminary evidence that the H1N1 Flu Vaccine Pandemrix can evoke immune system mediated damage to the orexin – hypocretin neurons and induce narcolepsy in individuals with a particular genetic variant. The orexin – hypocretin neurons were only recently discovered in the mid 1990s, by two separate research groups, hence, the two names for the same molecule. For this paper, we’ll be utilizing the orexin nomenclature.
Initially, the orexin neurons were thought to be involved only in feeding behavior, as damage elicited hypophagia in animals. Soon it was learned that more severe damage to the orexin neurons induced narcolepsy and the orexin system became a key focus in narcolepsy related research. With time, however, it became quite clear that these neurons were involved in regulating a myriad of hormone and neurotransmitter systems and their consequent behaviors. Narcolepsy or rather the ability to sustain wakefulness, is but one of the many functions regulated by the orexin system.
In a previous paper, I touched briefly on the possibility that the orexin neurons might be damaged and have diminished functionality in individuals suffering from post Gardasil side effects. In particular, I suspected these neurons were indicated in post-Gardasil hypersomnia, a derivative of narcolepsy. That may be only the tip of the iceberg. As I soon learned, the hypocretin/orexin neurons are brain energy sensors and may be involved in array of post medication or vaccine adverse reactions. Indeed, they may be central to the ensuing state of sickness behaviors that emanate once an organism becomes overwhelmed.
The Orexin – Hypocretin Basics
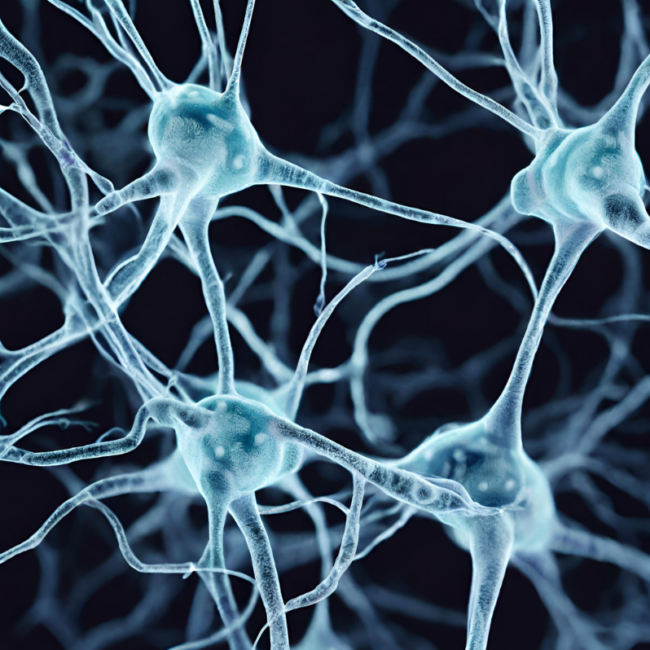
Orexin nuclei are located in the lateral hypothalamus, the section of the hypothalamus that is most known for regulating feeding, arousal and motivation. The hypothalamus is the master regulator for all hormone systems and hormone related activity including feeding, sleeping, reproduction, fight, flight, energy usage – basically every aspect of human and animal survival. It sits at the interface between the central nervous system functioning and the endocrine system functioning.
From the lateral hypothalamus, orexin neurons project across the entire brain with its two receptors (OXA and OXB) differentially distributed throughout the central nervous system and even in the body, including in the kidney, adrenals, thyroid, testis, ovaries and small intestine. The orexin neurons also modulate local networks of adjacent neurons within the hypothalamus that in turn influence a myriad of behaviors.
The most densely innervated brain regions include the thalamus, the locus coeruleus, dorsal raphe nucleus, accounting for the hormone’s role in arousal, feeding and energy management. At the most basic level, release of the orexin induces wakefulness. When orexin neurons are turned on and firing appropriately, arousal is maintained. When orexin neurons are turned off, diminished or dysfunctional, melatonin, the sleep promoting hormone, is turned on. The two work in concert to manage wakefulness and sleep.
Orexin receptors are also located in the amygdala, the ventral tegmental area (VTA) and throughout the limbic system, accounting for its role in emotion and the reward system. Orexin directly activates dopamine in the VTA. The VTA is the reward, addiction, and in many ways, the pleasure center of the brain. All drugs of addiction, all pleasurable activities, activate dopamine in the VTA. Through the release of dopamine, here and elsewhere, orexin modulates the motivation to sustain pleasurable activities. When orexin is diminished, not only does dopamine diminish, but the motivation to sustain behaviors decreases and dysphoria increases.
That’s not all. Orexin influences the release of many other neurotransmitters and hormones, several of which are co-located on the orexin neurons themselves. For example, the neuropeptide dynorphin is co-located on orexin neurons. Dynorphin is an endogenous opioid involved in the perception of pain and analgesia. It has dual actions that can both elicit analgesia or pain depending upon dose and length of exposure. Stress activates dynorphin. Dynorphin then inhibits orexin firing by as much as 50%. Illness is a stressor, a vaccine is a stressor, either could activate dynorphin and inhibit orexin. After the initial activation of dynorphin, and the ensuing decrease in orexin, the presence of chronic stressors and chronic pain could begin a continuous feedback loop of diminished arousal, and increasing pain.
Other Neurochemical Connections
- Consistent with orexin’s role in arousal, orexin neurons contain glutamate vesicles. Glutamate is the brain’s primary excitatory neurotransmitter. Drugs that increase glutamate, also increase orexin. Drugs that block glutamate, via its NMDA receptor, decrease orexin. Common migraine medications block glutamate and thereby may also diminish orexin.
- Serotonin and norepinephrine decrease hypocretin/orexin firing (suggesting if one is concerned with hypersomnia, anti-depressants might not be a good option).
- As one might expect, orexin neurons are inhibited by GABAα agonists – sedatives. From a women’s health perspective, consider that cycling hormones would also affect orexin neurons through the GABAα pathway. Progesterone is a GABAα agonist – a sedative, while DHEA and its sulfated partner DHEAS are GABAα antagonists, anxiolytics that block GABAα, reduce sedation, and thereby increase anxiety and wakefulness. There may be a cyclical nature to orexin firing that has yet to be investigated.
- The hypocretin/orexin neurons also influence galanin, a GI and CNS hormone that seems to inhibit the activity of a variety of other neurons in those regions.
These are but a few of the brain systems that the orexin neurons touch in some way or another. Damage to this system would have serious health consequences by initiating a cascade of biochemical changes within the brain and body. Many of which, we have yet to fully understand.
How Might the Orexin Neurons Become Inhibited?
Quite easily, apparently. In addition to the orexin’s vast interconnected pathways with a myriad of neurotransmitters and neuropeptides, the orexin neurons act as energy and activity sensors with some unique intracellular mechanics that make them especially sensitive to the changing dynamics of the extracellular milieu. Disruptions in ATP, glucose and temperature, elicit reactions in orexin functioning.
Orexin neurons require as much as 5-6X the amount of intracellular ATP to maintain firing, and to maintain a state of wakefulness or arousal. This extreme sensitivity to reduced ATP makes the orexin neurons uniquely positioned to sense and monitor brain energy resources, early, before ATP levels become critical in other areas of the brain. The orexin neurons cease firing when ATP stores become low, thereby allowing the reallocation energy, perhaps to those cells required for survival, breathing and heart rate. As Hans Selye observed many decades ago, one of the first, and indeed, most consistent of the sickness behaviors, no matter the disease, is lethargy, fatigue and sleepiness. Orexin is at the center of this behavior.
Orexin neurons react to extracellular glucose levels, though perhaps not as one might expect. When extracellular glucose levels are high, orexin neurons stop firing via what is called an inward rectifying potassium (K+) channel that is ATP dependent. That means that when extracellular glucose is high, intracellular ATP is allocated to open K+ channels and flood the cell with the inhibitory K+ ions. K+ hyperpolarizes the cell, prohibiting it from firing. This mechanism reminds me of Dr. Peter Attia’s talk about the nature of Type 2 Diabetes and our approach to treatment. He proposes that the body’s metabolic response – the conservation of energy – to Type 2 Diabetes is not something aberrant but is exactly as it should be with a disease state. We’re just not treating the correct disease state.
Another way we can shut down the orexin neurons is via increased temperature. The orexin neurons are very sensitive thermosensors. Increased temperatures shut down orexin firing via the inward K+ flow. Again, this is consistent with sickness behaviors and the reallocation of resources.
Orexin – Hypocretin Neurons in Migraine and Seizures
Diminished orexin has been linked to migraine and seizure activity. With migraines specifically, orexin may contribute to the early warning, hours to days, of impending cortical disruption via changes in feeding and sleep patterns that often precede migraine onset. Orexin may also be linked to the pre-migraine aura mediated by changes in brain electrical activity that prelude the migraine pain itself by minutes, called cortical spreading depression or more appropriately, cortical spreading depolarization – the massive spreading change in ion balance of the neurons. Initially the wave is excitatory, neurons are firing, but that is soon followed by a period of neural silence. Finally, orexin is also connected to the vasodilation of the trigeminal nerve, the nerve responsible for migraine pain. These findings have led some to call orexin a migraine generator.
Diminished cerebral spinal concentrations of oxerin have been found in patients generalized tonic-clonic seizures. Conversely, in rodent studies, injections of orexin elicit seizure activity. Despite the somewhat contradictory findings in seizure activity versus migraine activity, it is likely that the orexin system is involved both disease processes.
Pulling it all Together: Orexins Monitor and Mark Disruptions in Brain Homeostasis
Here’s where it gets really interesting. Although some have argued orexin, particularly diminished orexin functioning, is the cause and culprit of disruptions in brain homeostasis, leading to narcolepsy, excessive sleepiness, migraine, seizures and other diseases, I think this system represents merely a marker of a disease process. I think the orexin system is the stopgap, the final barrier of disrupted cellular energetics, of mitochondrial function. Mitochondrial ATP is the key.
When we consider orexin’s role in migraine, in particular, we see clearly how environmental changes (diet, stress, illness, medication/toxin exposure) can lead to changes in the extracellular milieu where orexins reside. The orexin sensors adjust to these changes, mostly by reducing neural firing in attempt to counteract damages. The reduction in orexin then elicits the premonitory phases of the impending brain disruptions, sleep and hypophagia – the sickness behaviors. If it progresses, the massive waves of electrical disruption ensue, and migraine, perhaps even seizures are evoked. When the extracellular environment become chronically disrupted, so too does the diminishment of orexin activity, thereby initiating a perpetuating loop of dysregulated brain activity. We can hypothesize that similar progressions exist with disease processes marked by aberrant electrical activity, such as epilepsy.
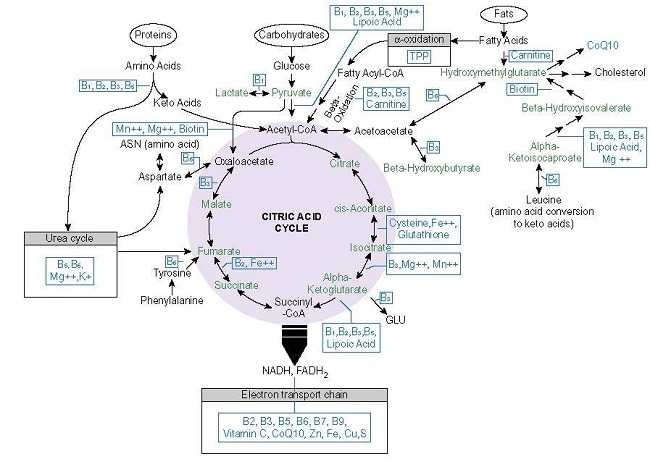
We know that mitochondrial dysfunction is often generated by genetic polymorphisms and can predispose individuals to an array of seemingly unrelated conditions like migraine and fibromyalgia, dysautonomias and cognitive deficits. At the root of the dysfunction is a error of some sort in mitochondrial energy processing – ATP.
What has become increasingly clear, is that the production of cellular energy, can be disrupted environmentally, by diet, illness and exposures, if co-factors necessary for the production ATP like thiamine are diminished. It is via diminished ATP production, that I think some medications and vaccines evoke adverse reactions in some individuals. The orexin system, because it is so exquisitely sensitive to changes in cellular energy, is our warning system; first by subtle changes in neurochemistry, then by changes in arousal and feeding behavior, and finally, by an all-out reallocation of resources – excessive sleeping. If ATP remains deficient chronically, and an individual is so disposed, then the cortical misfiring we see in migraine and seizure ensues, along with autonomic dysregulation and the syndromes associated therewith. It is not the orexin – hypocretin system that is at root of many of these diseases, but rather, the causes are deeper yet and reside with mitochondrial health.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image created using Canva AI.
This article was published originally on January 29, 2014.