In this article, we will briefly examine some of the reasons why supplementing with the mineral magnesium is often essential when repleting thiamine, and also when using higher doses to support health conditions. In a minority of people, intolerance of magnesium supplements might be resolved when using thiamine simultaneously.
First of all, thiamine and magnesium are closely paired biochemically speaking. Magnesium is either directly or indirectly involved in the activity of numerous thiamine-dependent enzymes. Importantly, the activation of thiamine inside the cell greatly depends upon sufficient magnesium stores.
Thiamine Activation Requires Magnesium
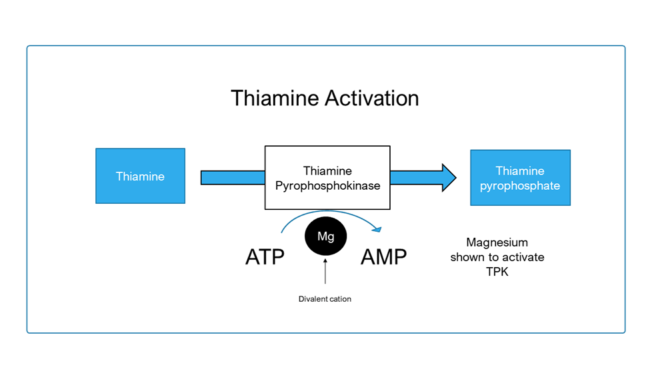 After absorption, dietary forms of thiamine gain entry into the cell through transport proteins. Once inside, free thiamine must be converted (or “activated”) into thiamine pyrophosphate (TPP), the biochemically active coenzyme form. This is achieved by an enzyme called thiamine pyrophosphokinase, which removes a phosphate from adenosine triphosphate (ATP) and attaches it to thiamine to make TPP. This enzymatic reaction has been shown to require a divalent cation, which in most cases is magnesium.
After absorption, dietary forms of thiamine gain entry into the cell through transport proteins. Once inside, free thiamine must be converted (or “activated”) into thiamine pyrophosphate (TPP), the biochemically active coenzyme form. This is achieved by an enzyme called thiamine pyrophosphokinase, which removes a phosphate from adenosine triphosphate (ATP) and attaches it to thiamine to make TPP. This enzymatic reaction has been shown to require a divalent cation, which in most cases is magnesium.
This is especially important when using supplements with the aim of rapidly increasing intracellular thiamine levels, because the above “activation” process will increase the requirement for magnesium. Without enough magnesium to meet this demand, it is at least theoretically plausible that there will be less active TPP which can be utilized.
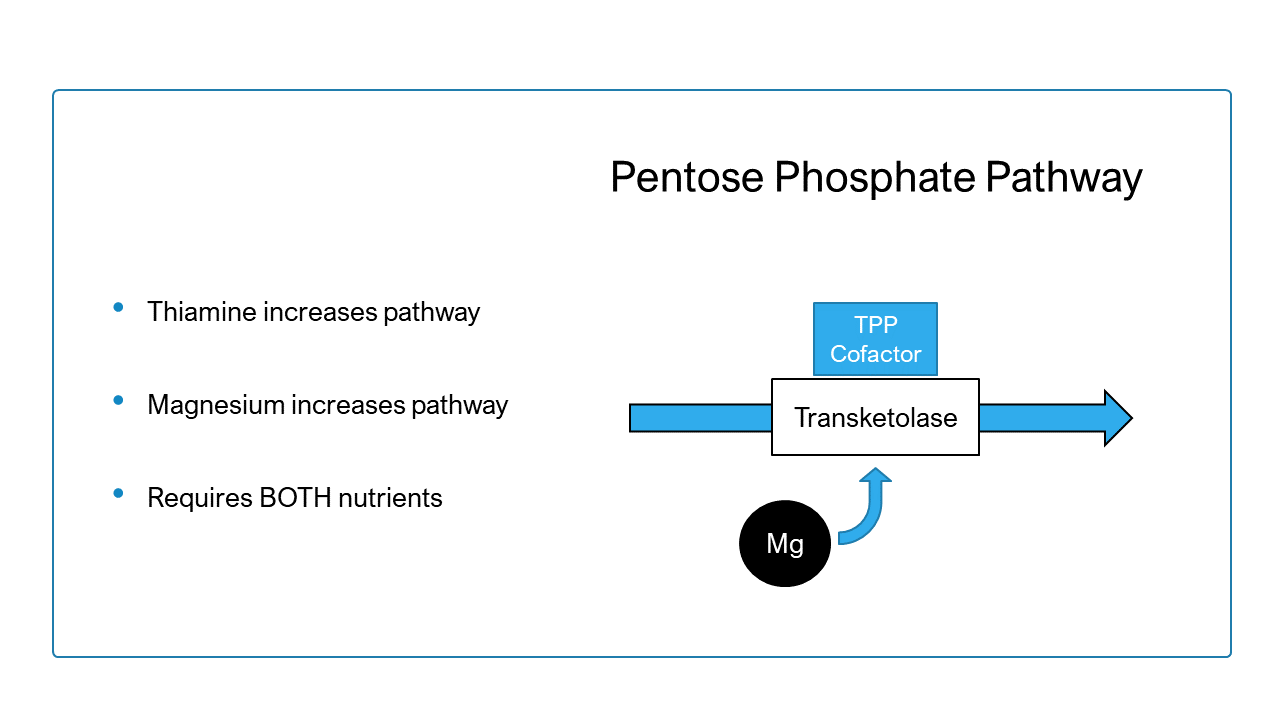
The Transketolase Enzyme
Likewise, the transketolase enzyme located within the pentose phosphate pathway also requires magnesium to undertake its activities. Research has shown that both magnesium and thiamine alone are capable of increasing transketolase activity.
Alpha-ketoglutarate Dehydrogenase and Pyruvate Dehydrogenase
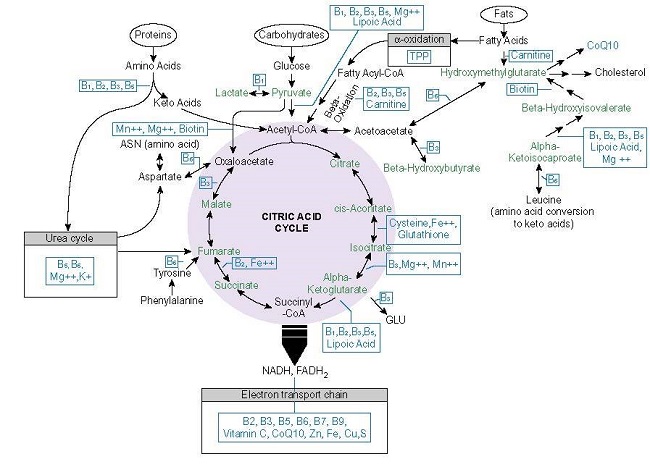
Magnesium ions were shown to directly increase the activity of the thiamine-dependent rate-limiting alpha-ketoglutarate dehydrogenase complex (KGDH), an enzyme unit involved in the Krebs cycle (part of the larger process of generating cellular energy). Research indicates that KGDH requires both TPP and magnesium for maximal activity.
Furthermore, a similar thiamine-dependent enzyme complex positioned at the interface between glycolysis and the Krebs cycle called the pyruvate dehydrogenase complex (PDHC) also requires magnesium, but indirectly. The PDHC is essential for carbohydrate metabolism. Although magnesium ions do not directly interact with the PHDC, they do exert significant influence on a related regulatory enzyme called pyruvate dehydrogenase phosphate phosphatase (PDHP). Magnesium activates PDHP, and PDHP is responsible activation of the PDHC. Hence, thiamine directly increases PDHC activity, and magnesium indirectly increase it as well.
Thiamine and Magnesium Should Be Supplemented Together
With the numerous interrelated roles of these two nutrients taken into consideration, is it any wonder that research has demonstrated negative consequences of supplementing one without the other?
One animal study showed that thiamine supplementation in magnesium-deficiency (and/or sulfate deficiency) resulted in reduced thiamine concentrations in liver and elevated triglycerides, suggesting a role for magnesium in liver retention of thiamine. Another study looking at thiamine supplementation in magnesium deficient animals found that the addition of thiamine results in a significant decrease in blood and bone concentrations of magnesium, which indicates an increased demand for magnesium and depletion of the stored mineral. The same study showed a lower levels of thiamine in nerve, liver, and kidney of magnesium deficient animal, providing further support for magnesium’s role in thiamine retention. Additionally, they showed that thiamine could not increase transketolase activity in the presence of magnesium deficiency.
Correcting Wernicke Encephalopathy, the end stage neurological consequence of severe thiamine deficiency with thiamine alone was found to be ineffective in one case report, and only after correcting hypomagnesaemia (addressing magnesium deficiency) did the patient’s transketolase normalize and symptoms resolve. A more recent report showed the same results.
So to conclude, it is clear that magnesium is absolutely essential for normal thiamine activity in the body, and one should take great care to ensure sufficient intake when addressing underlying thiamine issues. This is especially important when consistently using high doses.
Magnesium and Thiamine
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image created using Craiyon.com
This article was published originally on October 25, 2021.