Diethylstilbestrol (DES) is a synthetic estrogen. Known as DES in the United States, it is more commonly known as stilboestrol in the UK and Australia. It was the first synthetic estrogen produced, developed by Sir E. Charles Dodds and colleagues in the UK in 1938.
Constructed from a chemical base, it produced the same feminizing effect as estrogens derived from animals (e.g. Premarin) but was more powerful and cheaper to produce. DES cost about two dollars per gram to produce compared to the three hundred dollars to produce natural estrogen.
Never patented, the DES formula was published in the magazine Nature on 15 February 1938, giving the world the first cheap and powerful estrogen. As it was never patented, within months drug companies around the world were working with this formula, vying to market this lucrative new product straight out of the lab.
This has been likened to opening Pandora’s Box, an action that turns out to have detrimental, unintended and far-reaching negative consequences.
Dodds was aware of what a powerful and potentially carcinogenic drug he had synthesised. In the months following the discovery, Dodds became increasingly concerned about the carcinogenicity of the newly synthesized drug. In his laboratory he noticed that men on his staff who handled and inhaled the stilboestrol powder were growing breasts, suggesting to him stilboestrol might cause breast cancer in men. He suggested that animal studies be carried out looking at the carcinogenicity of stilboestrol in male rodents. In 1940 a paper was published showing that stilboestrol caused mammary cancers in both male and female mice.
Many studies of a variety of experimental, agricultural and domestic animals were conducted in the 1940s and showed serious adverse effects of the drug including cancer, fetal death, and sterility of offspring.
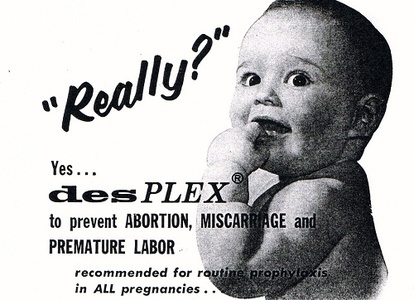
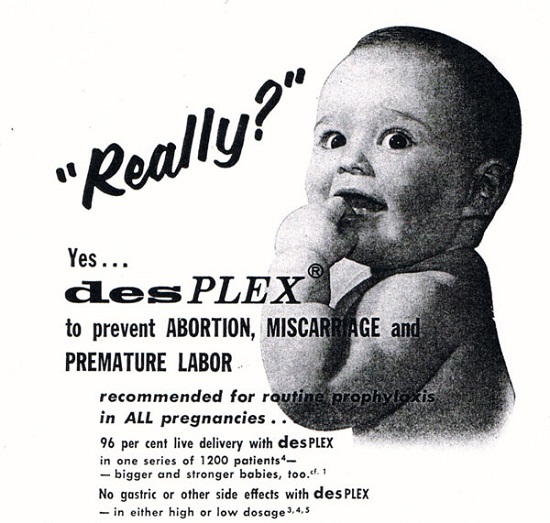
Dodds never envisaged that stilboestrol would be given to healthy women and was against the automatic and “promiscuous” prescribing of estrogen: He was aghast when told it was being used to “prevent miscarriage”; particularly as he had conducted research showing the drug could prevent or end pregnancies in rabbits and rats. This made it a potential birth control or emergency contraceptive pill. However, Dodds said that the human female reproductive cycle was too delicate to introduce foreign substances into it, and he denounced the use of DES to prevent or end pregnancies.
The risk of cancer with these drugs was well known and documented. In fact Dodds himself spent many years thereafter warning that these drugs put women at serious risk of endometrial and breast cancer.
However it was all too late – Pandora’s Box was well and truly open.
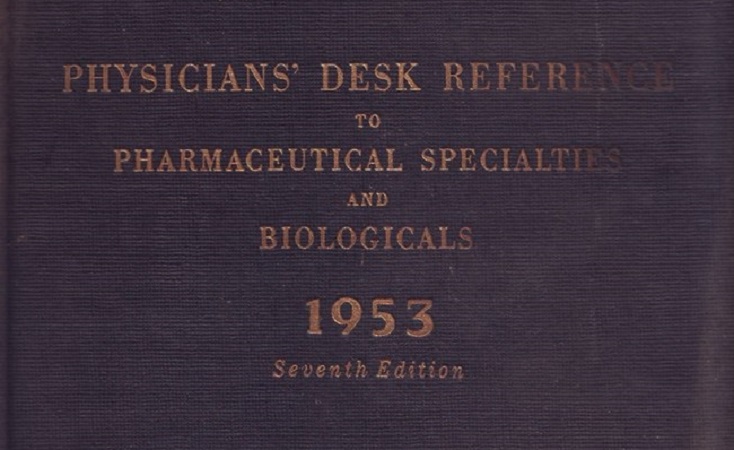
Despite the controversy and warnings, the Age of estrogen had well and truly begun. Over the following decades, DES and other exogenous estrogens were marketed and prescribed for a bewildering, often contradictory, range of conditions: to slow and prevent aging; to stop hot flushes and as treatment for other menopausal symptoms; to prevent miscarriage, for pregnancy maintenance, as a pregnancy “tonic”; as the oral contraceptive pill; as the ‘morning after’ contraceptive pill; to stunt the growth of tall girls; to suppress lactation; as a hormonal pregnancy test; to treat acne…
What these uses have in common is that they were experimental; they often didn’t work; and they were never proven safe, frequently having serious, often unexpected, long-term health outcomes for those exposed to the drugs.
And, despite Dodds’ concern, it was healthy women who were “automatically and promiscuously” prescribed the drugs.
To quote Barbara Seaman from The Greatest Experiment Ever Performed on Women: Exploding the Estrogen Myth (2003),
I call the marketing, prescribing, and sale of these drugs an experiment because, for all these years, they have been used, in the main, for what doctors and scientists hope or believe they can do, not for what they know the products can do. Medical policy on estrogens has been to ‘shoot first and apologise later’ – to prescribe the drugs for a certain health problem and then see if there is a positive result.
It wasn’t until 1971 that the magnitude of the adverse effects of stilboestrol use started to emerge. DES emerged as a public health crisis in 1971 with the discovery of the ‘DES Cancer’, an aggressive, clear cell adenocarcinoma of the cervix/vagina, in DES daughters.
The discovery of this “biological time bomb” sent shock waves through the medical science community. Up until that time, based on the Thalidomide experience, it was thought any adverse effects of a drug given during pregnancy would show up immediately as “birth defects”. It was obvious that DES was a whole new ball game.
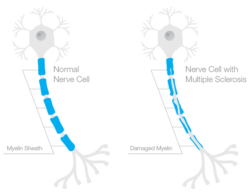
This lead to a paradigm shift and DES was recognized as an endocrine disruptor. Prenatal exposure to an endocrine disruptor such as DES results in multiple, diverse serious effects that are latent and delayed, being manifest years after the original exposure.
However, it was the Australian study of Tall Girls that moved our understanding of endocrine disruption to a new level. The small study was truly groundbreaking and far-reaching in the implications of its findings. No one had ever researched the long-term effects of exposure to an endocrine disruptor at this critical time of development, i.e. puberty. Another important feature of this study is that while DES was initially used, it was replaced in the mid-1970s (probably as a result of the ‘DES cancer’ being discovered) by ethinyl estradiol. So a very important ‘incidental’ finding of this study is that ethinyl estradiol, the estrogen found in the oral contraceptive pill, is an endocrine disruptor.
An important paper published from this study showed that tall girls treated with estrogen in early adolescence were nearly twice as likely to experience unexplained infertility as adults when compared to the matched control group of untreated tall girls.
This finding was replicated and extended in a 2011 Dutch study that evaluated fertility and ovarian function. Interestingly the European treatment for tall girls was high doses of synthetic estrogen (ethinyl estradiol) in combination with cyclic progestin. The impact of treatment on impaired fertility was even more pronounced than that observed in the Australian study. In terms of ovarian function, treated women were more likely of being diagnosed with premature ovarian failure.
A 2014 Swedish study found that the tall girl treatment regime was associated with an increased risk of melanoma.
Allied to this was the realization that DES causes epigenetic changes, resulting in the next and subsequent generations potentially being affected. Epigenetics refers to heritable traits in cells and organisms that do not involve changes to the underlying DNA sequence. Scientists believe that DES, as an endocrine disruptor, impairs and changes the normal pattern of gene expression i.e. when genes are turned on and off. It is thought that exposure to DES dysregulates the epigenome, with potential consequences for subsequent developmental disorders and disease manifesting in childhood, over the life course, or transgenerationally.
So DES is not only the first exogenous estrogen to be synthesized; it is the first compound to be recognized as an endocrine disruptor; and it is the primary model for environmental endocrine disrupting chemicals. In addition, it can be seen that DES is the primary model for pharmaceutical endocrine disrupting drugs.
Thus, the DES exposed are the ‘canaries in the coalmine’, the harbingers of the future.
Nearly 80 years ago Sir Charles Dodds inadvertently opened Pandora’s Box and we are still experiencing the unintended effects all these years later.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image: Vicious Bits/Flickr CC2.0
This article was published originally on July 24, 2017.


































 DES is not something of the past. People who have been exposed to this drug years ago are battling with health issues and fighting for their lives as I’m writing this blog post. Who knows what health problems the grandchildren of the mothers who were prescribed this drug will have to deal with as they grow up. I want my daughters to receive adequate medical care and monitoring if they ever have to suffer the consequences of this drug. This is why together with my husband we support the great work done by the very few International DES Action Groups who are providing valuable information and are advocating for the DES victims.
DES is not something of the past. People who have been exposed to this drug years ago are battling with health issues and fighting for their lives as I’m writing this blog post. Who knows what health problems the grandchildren of the mothers who were prescribed this drug will have to deal with as they grow up. I want my daughters to receive adequate medical care and monitoring if they ever have to suffer the consequences of this drug. This is why together with my husband we support the great work done by the very few International DES Action Groups who are providing valuable information and are advocating for the DES victims.



